Completing 18 Years of Delivering Smiles...Thank You Everyone Associated With Aesthetic Dental Clinic for Being with Us in Our Wonderful Journey.
Facial trauma is an injury of the face. It may include the facial bones such as the upper jaw bone (maxilla).
Causes
 Facial injuries can affect the upper jaw, lower jaw, cheek, nose, eye socket, or forehead. They may be caused by blunt force or be the result of a wound.
Common causes of injury to the face include:
Facial injuries can affect the upper jaw, lower jaw, cheek, nose, eye socket, or forehead. They may be caused by blunt force or be the result of a wound.
Common causes of injury to the face include:
Car and motorcycle crashes
Wounds
Sports injuries
Violence
Symptoms
Symptoms may include:
Changes in feeling over the face
Deformed or uneven face or facial bones
Difficulty breathing through the nose due to swelling and bleeding
Double vision
Missing teeth
Swelling or bruising around the eyes that may cause vision problems
Exams and Tests
 The health care provider will perform a physical exam, which may show:
The health care provider will perform a physical exam, which may show:
Bleeding from the nose, eyes, or mouth
Nasal blockage
Breaks in the skin (lacerations)
Bruising around the eyes or widening of the distance between the eyes, which may mean injury to the bones between the eye sockets
Changes in vision or the movement of the eyes
Improperly aligned upper and lower teeth
The following may suggest bone fractures:
Abnormal feelings on the cheek
Irregularities of the face that can be felt by touching
Movement of the upper jaw when the head is still
Can you What causes the jaw to lock?
Grinding or clenching your teeth, which puts a lot of pressure on the joint. Movement of the soft cushion or disc between the ball and socket of the joint. Arthritis in the joint. Stress, which can cause you to tighten facial and jaw muscles or clench the teeth.
Can TMJ give you headaches?
 Temporomandibular joint disorder, or TMD, causes jaw pain that may be mistaken for recurring tension headaches according to a recent study of TMJ symptoms. Jaw pain due to TMJ symptoms will not respond to tension headache treatment. Instead, such pain must be treated in the same way traditional TMJ symptoms.
Temporomandibular joint disorder, or TMD, causes jaw pain that may be mistaken for recurring tension headaches according to a recent study of TMJ symptoms. Jaw pain due to TMJ symptoms will not respond to tension headache treatment. Instead, such pain must be treated in the same way traditional TMJ symptoms.
What is TMJ and what causes it?
When this joint is injured or damaged, it can lead to a localized pain disorder called temporomandibular joint (TMJ) syndrome. Causes of temporomandibular joint (TMJ) syndrome include injury to the teeth or jaw, misalignment of the teeth or jaw, teeth grinding, poor posture, stress, arthritis, and gum chewing.
What causes a clicking jaw?
The most common symptom of TMD is pain in the joint itself or the chewing muscles that attach to it. ... A painful grinding or popping in your joint can be a warning, of course, but a clicking sound in your jaw or limited movement "without pain" isn't always an indication of a TMJ problem, nor does it need treatment.
What is TMJ and how is it treated?
TMJ Syndrome Overview. Temporomandibular joint (TMJ) syndrome is pain in the jaw joint that can be caused by a variety of medical problems. The TMJ connects the lower jaw (mandible) to the skull (temporal bone) in front of the ear. ... You have two TMJs, one on each side of your jaw.
What causes TMJ syndrome?
 TMJ disorders a type of temporomandibular disorder or TMD can cause painin your jaw joint and in the muscles that control jaw movement. The exact cause of a person's TMJ disorder is often difficult to determine. Your pain may be due to a combination of factors, such as genetics, arthritis or jaw injury.
TMJ disorders a type of temporomandibular disorder or TMD can cause painin your jaw joint and in the muscles that control jaw movement. The exact cause of a person's TMJ disorder is often difficult to determine. Your pain may be due to a combination of factors, such as genetics, arthritis or jaw injury.
What is a TMJ disorder?
TMJ Disorders. Main Content. Temporomandibular joint and muscle disorders, commonly called "TMJ," are a group of conditions that cause pain and dysfunctionin the jaw joint and the muscles that control jaw movement.
What causes pain in the jaw?
Temporomandibular disorder, also known as TMD, affects the temperomandibular joint of the jaw. In addition to pain, this disorder can cause the jaw to make a clicking sound when opening the mouth or chewing. In severe cases, the disorder can even cause the jaw to become permanently stuck in an open or closed position.
How are you diagnosed with TMJ?
 If your doctor or dentist suspects a problem with your teeth, you may need dental X-rays. A CT scan can provide detailed images of the bones involved in the joint, and MRIs can reveal problems with the joint's disk. TMJ arthroscopy is sometimes used in the diagnosis of a TMJ disorder. ... Temporomandibular joint pain
If your doctor or dentist suspects a problem with your teeth, you may need dental X-rays. A CT scan can provide detailed images of the bones involved in the joint, and MRIs can reveal problems with the joint's disk. TMJ arthroscopy is sometimes used in the diagnosis of a TMJ disorder. ... Temporomandibular joint pain
Why does it hurt my jaw to chew?
Possible causes of TMD include: clenching your jaw or grinding your teeth during sleep (bruxism) which overworks the jaw muscles and puts pressure on the joint (often caused by stress) wear and tear of the inside of the jaw joint usually caused by osteoarthritis.
In early pregnancy, different parts of a babys face develop separately and then join together. If some parts do not join properly, the baby is born with a cleft.
A cleft lip and/or palate is the most common craniofacial abnormality, which is a problem to do with the skull and face.
 A cleft lip can range from a little notch in the coloured part of the lip to a complete separation of the upper lip which can extend up and into the nose. This can affect one side of the mouth (unilateral) or both sides (bilateral), and can be complete (meaning the cleft goes up into the nose) or incomplete.
A cleft lip can range from a little notch in the coloured part of the lip to a complete separation of the upper lip which can extend up and into the nose. This can affect one side of the mouth (unilateral) or both sides (bilateral), and can be complete (meaning the cleft goes up into the nose) or incomplete.
A cleft lip can also affect the gum where the teeth come through. Again, this can range from a small notch to a complete separation of the gum into two parts.
A cleft palate is a gap in the roof of the mouth. The back of the palate (towards the throat) is called the soft palate, and the front (towards the lips) is called the hard palate. A cleft can affect the soft palate or both the soft and hard palate.
Sometimes a baby with a cleft palate may have a small lower jaw (mandible) and a few babies with this combination may have difficulties with breathing. This condition may be identified as Pierre Robin Sequence.
You can have a cleft lip, a cleft palate, or a cleft lip and palate. A cleft palate by itself is often called an isolated cleft palate.
What causes cleft lip and palate?
No one knows exactly what causes a cleft. Research tells us its often caused by a combination of different genetic and environmental factors.
 Genetics is all about things inherited from family members, like eye and hair colour. With a cleft, sometimes there is a clear family link, other times it just happens as a one off.
Genetics is all about things inherited from family members, like eye and hair colour. With a cleft, sometimes there is a clear family link, other times it just happens as a one off.
Environmental factors mean things that happen just before or during pregnancy, like taking a certain medicine or how the baby starts growing in the womb. Most of the time, a cleft is caused by genetic and environmental factors coming together in a way which cant be predicted or prevented. If you have a child with a cleft, it is very unlikely to be because of something you did or did not do.
Sometimes a cleft is caused by part of a syndrome, which is when lots of different symptoms happen together. If you want to find out more about what caused your or your childs cleft, the Clinical Geneticist in your Cleft Team might be able to help you.
How many people have a cleft?
Around one in 700 babies are born with a cleft around the world. Thats around 1,200 babies born with a cleft each year in the UK! Of these, around 45% will have an isolated cleft palate, 24% will have an isolated cleft lip, and 31% will have a cleft lip and palate. Bilateral cleft lip and palate is the least common type, at just 9%.
How is it treated?
Aesthetic Dental Clinic is made up of a number of specialists from surgeons to speech therapists dedicated to providing the best possible care for people born with a cleft, from infancy through to adulthood.
 Surgery is needed to close the gap left by the cleft. This will usually happen when the child is under a year old.
Surgery is needed to close the gap left by the cleft. This will usually happen when the child is under a year old.
Every cleft is unique, just like every child, so the exact treatment pathway will vary. It may include further surgery to help with issues such as speech and growth of adult teeth. It may also include speech therapy, help with hearing, orthodontic work, etc.
What are Jaw Cysts?
A cyst is a sack or pouch which forms within tissues and contains fluid. This cyst is not a cancerous growth.
Cysts can develop in many places in the body. Around the face and mouth they can develop under the skin, under the mouth lining, within the saliva glands, and within the jawbones.
There are several different types of cysts within the jawbones. The commonest type is called a periapical cyst. These develop around the roots of teeth usually as a result of a chronic infection. Other cysts can develop around an uninterrupted tooth such as a wisdom tooth. These are called dentigerous cysts. The final common group of jaw cysts develop from cells that form teeth. These are known as odontogenic cysts.
Jaw cysts grow very slowly and in the vast majority of cases patients do not have any symptoms. They are often discovered as an incidental finding when x-rays are taken to look for other things. If the cyst becomes infected they can become painful. Cysts can grow very large and can cause damage to adjacent teeth which can become loose. Very large cysts can also expand the jaw and very occasionally can be so big that they can weaken the jaw leading to a fracture.
What will happen at the consultation?
The consultation is a very important part of the treatment, it is an opportunity to meet the consultant and team that will be looking after you. Following an examination and x-rays the consultant will be able to establish a diagnosis. Sometimes when cysts are large or close to other structures it may be necessary to obtain a CT scan which gives a 3-D view and aids the surgery. The consultant will explain what the surgery will entail and what to expect afterwards.
How are jaw cysts removed?
The treatment for cysts is to remove them. This is done by a small incision inside the mouth and removal of part of the bone. Occasionally when cysts are very large it is possible to treat them by surgical decompression. Following the surgery the cyst is sent to a specialist pathologist for examination under a microscope to confirm the diagnosis.
What type of anaesthetic will be used?
Your consultant will discuss the type of anaesthetic appropriate to your case, taking into account your general health and your previous experiences of having dental treatment. In many cases treatment can be carried out under local anaesthetic with you awake, but your teeth and jaw will be numbed. You may be advised or wish to have the procedure undertaken under a general anaesthetic. This will involve admission to hospital, usually as a day case, and means you will be asleep during the procedure.

Preparing to have your Jaw Cyst removed
Your consultant will explain how to prepare for your procedure. For example, if you smoke, you will be advised to stop as this significantly increases your risk of wound infection, slowing your recovery. Some types of medication you take may also require special consideration.
If you are having a local anaesthetic then you can eat and drink as normal beforehand though we advise that you keep the meals light. Any medication you are taking can be continued unless you are specifically instructed otherwise. You can even drive to and from your appointment though it is usually best (and nice) to bring a friend or relative with you.
If you are having a general anaesthetic, you will be asked to follow fasting instructions, this means not eating or drinking for some hours prior to the procedure. You will be given specific instructions by the hospital prior to your admission date.
During your consultation the consultant will also explain any risks or complications that can arise from treatment and how they can best be avoided or managed. Your surgeon will give you ample opportunity to ask any questions you may have and ensure that you are happy for the procedure to go ahead. If you are then you will be asked to give your informed consent by signing a consent form detailing the procedure agreed and any specific complications discussed.
What happens after surgery?
You will need to rest until the main effects of the anaesthetic (local or general) have worn off.
After a local anaesthetic you will usually be able to go home straight after the procedure has been carried out. It may take a while before the feeling comes back to your jaw so it is best to avoid eating or drinking during this period as you could easily bite your lip or cheek or burn yourself on something hot, as you will not have your normal protective pain reflexes.
If you had a general anaesthetic or sedation you will need to stay longer and arrange for someone to drive you home. You should also have a friend or relative stay with you for the first 24 hours in case you experience problems and need help.
Your consultant will give you advice about looking after your mouth when you go home and suitable pain medication and appropriate antibiotics or mouthwashes to take home. You may also be given a date for a follow-up appointment.
Dissolvable stitches will disappear on their own in seven to 10 days. Non-dissolvable stitches are removed around a week after surgery.
Recovery from your procedure
You should expect some discomfort. If you need them, you can take over-the-counter painkillers such as Paracetamol or Ibuprofen. Follow the instructions in the patient information leaflet that comes with your medicine and ask your pharmacist for advice. Do not take Aspirin because this can make any bleeding worse. Avoid any medication that you have a known or suspected allergy to.
Do not vigorously rinse out your mouth during the first 24 hours. After 24 hours you can rinse gently after meals with warm salt water (half a teaspoon of table salt dissolved in a glass of water).
You should brush your teeth as usual, but keep your toothbrush away from the healing wound for the first couple of days.
To begin with, you should eat soft foods, gradually returning to your usual diet once your jaw feels more comfortable. You may have some facial swelling, bruising, pain or jaw stiffness for up to two weeks. These symptoms are usually at their worst for the first two or three days and then gradually improve.
Most people do not experience any significant problems after having their cyst removed. However contact your dentist, your GP, or us immediately if you develop any of the following symptoms:
bleeding that does not stop after applying pressure
difficulty in breathing or swallowing
severe pain that is not helped by painkillers
a high temperature
increasing swelling
Risks & Complications
Jaw Cyst removal is commonly performed and generally safe. However, in order to make an informed decision and give your consent, you need to be aware of the possible side effects and the risk of complications from this procedure. Most of these are the unwanted, but mostly temporary, effects of a successful treatment, for example feeling sick as a result of a general anaesthetic, swelling or bruising but can include more significant problems such as:
Bleeding
Infection
Accidental damage to other teeth and your jaw during your operation
Numbness in your lower lip or tongue, or changes to taste - this can be caused by nerve damage and there is a small chance that this could be permanent
Jaw stiffness - it's possible that you may not be able to open your mouth fully for a while.
The exact risks will differ for every person and some may be more specific to your case. This is why the initial consultation is so important, your consultant will be able to assess the risks for you and advise you accordingly. In summary, cyst removal is a common and safe procedure. Whilst it is natural to have some anxiety about having this done, careful assessment and removal by our experts will alleviate you of the problems you are having whilst minimising any risks to you.
Because the condition can develop anywhere inside your mouth, it can manifest in your jaw as well. Jaw cancer can occur either on the upper jaw, known as the maxilla; or the lower jaw, known as the mandible. If you experience any of the following jaw cancer symptoms, be sure to seek an evaluation by your dentist.
Jaw pain
A tumor is one explanation for pain in the jawbone, and this pain can make it hard for you to eat and chew. Jaw pain can develop for multiple reasons related to oral cancer, but it is one of the main symptoms associated with metastatic growths in the oral cavity, according to the National Institutes of Health (NIH). Metastatic tumors develop when cancer from one part of your body spreads to another, such as the maxilla or mandible.
Lumps on the jaw
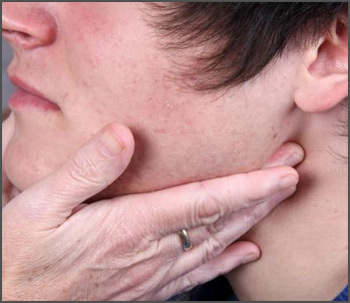 Lumps on the roof of your mouth or along your gumline may be the only jaw cancer symptoms you experience. These lumps can be a sign that cancer is developing on the jawbone beneath the mouth's soft tissues. If you notice a new lump inside your mouth and it doesn't resolve itself in two weeks, you need to see your dentist.
Lumps on the roof of your mouth or along your gumline may be the only jaw cancer symptoms you experience. These lumps can be a sign that cancer is developing on the jawbone beneath the mouth's soft tissues. If you notice a new lump inside your mouth and it doesn't resolve itself in two weeks, you need to see your dentist.
Swelling of the jaw
Swelling in the jaw is the most common symptom of osteosarcoma as a type of bone tumor that can affect the jaw. This swelling may be visible on the side of your face, but it can also occur inside your mouth. The roof of your mouth may be swollen as well, or you may notice swelling beneath your teeth depending on the location of the tumor. This inflammation is caused by the growth of the tumor inside the bone, and if it leads to gum irritation, your dentist may recommend using a toothbrush with extra-soft bristles.
Tooth mobility
Tumors in the jawbone can also lead to unexplained tooth mobility. If you notice that your teeth are loose or suddenly shifting positions, don't hesitate to let your dentist know. Tooth mobility could be caused by a tumor on your jawbone that is pushing your teeth out of place.
Pain, swelling, lumps on the jaw and loose teeth are all realistic jaw cancer symptoms. If you experience any of them, make sure to see your dentist right away for a screening to catch this treatable condition before it metastasizes.
Corrective jaw, or orthognathic surgery is performed by an oral and maxillofacial surgeon (OMS) to correct a wide range of minor and major skeletal and dental irregularities, including the misalignment of jaws and teeth. Surgery can improve chewing, speaking and breathing. While the patient's appearance may be dramatically enhanced as a result of their surgery, orthognathic surgery is performed to correct functional problems.
Following are some of the conditions that may indicate the need for corrective jaw surgery:
Difficulty chewing, or biting food
Difficulty swallowing
Chronic jaw or jaw joint (TMJ) pain and headache
Excessive wear of the teeth
Open bite (space between the upper and lower teeth when the mouth is closed)
Unbalanced facial appearance from the front, or side
Facial injury
Birth defects
Receding lower jaw and chin
Protruding jaw
Inability to make the lips meet without straining
Chronic mouth breathing
Sleep apnea (breathing problems when sleeping, including snoring)

Your dentist, orthodontist and OMS will work together to determine whether you are a candidate for corrective jaw, or orthognathic, surgery. The OMS determines which corrective jaw surgical procedure is appropriate and performs the actual surgery. It is important to understand that your treatment, which will probably include orthodontics before and after surgery, may take several years to complete. Your OMS and orthodontist understand that this is a long-term commitment for you and your family, and will try to realistically estimate the time required for your treatment.
What are Face Defects / Deformities?
Face Defects / Deformities, also known as Facial Defects / Deformities are deformities in the growth of the skull and facial bones. These are congenital deformities (present at birth) and can be corrected by reconstructive surgery. Face Defects / Deformities can be Craniofacial Deformities (affecting the skull), Maxillofacial Deformities (affecting the upper jaw) and Dentofacial Deformities (affecting the bony structure and teeth).
What are the different types of Face Defects / Deformities?
Cleft Lip - Cleft Lip or Hare Lip is a birth defect where the upper lip is split or separated either in the middle, on one side or on both the sides.
Cleft Palate - Cleft Palate is a condition when there is a cleft or a gap in the palate or the hard part of the roof of your mouth
Facial Cleft - This is a rare Face Defect / Deformity where a bone or skin in the middle of the face may be missing.
Craniosynostosis - This is a congenital Face Defect where the sutures (fibrous joints) of the skull bones fuse inappropriately and prematurely.
Plagiocephaly - In this type of Face Defect / Deformity, the forehead and the brow stop growing. This Face Defect / Deformity produces a flattening of the forehead and the brow on the affected side while the forehead on the opposite side tends to be excessively prominent.
Brachycephaly - This type of Craniofacial Deformity refers to a wide and high forehead region to be wide and high and the eyes may appear wide apart.
Trigonocephaly - In this type of Face Defect / Deformity, the forehead looks pointed, like a triangle, with closely placed eyes. This Face Defectoccurs due to closure of a suture that runs from the top of the head down the middle of the forehead, toward the nose.
This type of Face Defect / Deformity occurs when the suture that runs front to back, down the middle of the top of the head fuses prematurely. As a result, the shape of the skull becomes long and narrow. The skull is long from front to back and narrow from ear to ear.
Facial Palsy - This occurs due to paralysis of the facial nerve. In this kind of Face Defect, there is loss of control over facial expressions.
Chin Deformity - In this type of Face Defect / Deformity the chin is unusually small (mirognathia) or may be unusually large (macrognathia)
Upper Jaw (Maxillary) Deformity - One of the most common type of Upper Jaw (Maxillary) Deformity is called vertical maxillary excess. In this Facial Defect,there is excess bone of the upper jaw, the face appears long, the chin is recessed and the nose large in the profile view.
Lower Jaw (Mandibular) Deformity - There are two most common mandibular deformities; mandibular excess (protrusion) and mandibular deficiency (retrusion).
Deformational Plagiocephaly - This refers to asymmetrical shape of the head from repeated pressure to the same area of the head. This kind of Craniofacial Deformity usually results from keeping the infant's head in one position for long periods of time or it also be due to torticollis which is persistent tilt of the head to one side.
Vascular Malformations - Also known as lymphangioma, anteriovenous malformations or vascular gigantism. Vascular malformations are present at birth and increase in size as the child grows.
Hemangiomas - Also unknown as port wine stain, strawberry Hemangiomas and salmon patch. These are also called birth marks and mostly are present at birth (congenital).
'
Hemifacial Microsomia - In this Face Defect, the soft tissues and bones of the ear, mouth and jaw areas on one side of the face are under developed.
Microtia - In this Facial Deformity, the ear on one or both sides does not grow properly and may be accompanied by atresia of the ear canal.
Facial reconstruction is a method used in the forensic field when a crime involves unidentified remains. Facial reconstruction is usually performed by a sculptor who is an expert in facial anatomy. This sculptor could be a forensic artist but its not a requirement. Either way, the sculptor will work with forensic anthropologists to interpret the features of the skeleton that will ultimately help reveal the age, sex and ancestry of the victim. The sculptor can also reveal anatomical features (features that are related to the body structure) such as facial asymmetry, evidence of injuries like a broken nose or teeth that were lost before death. These factors are determined by using either the three-dimensional reconstruction technique or a two dimensional reconstruction technique.
What is facial reconstructive surgery?
Reconstructive surgery is, in its broadest sense, the use of surgery to restore the form and function of the body; maxillo-facial surgeons, plastic surgeons and otolaryngologists do reconstructive surge.
Why is facial reconstruction important?
Facial recognition and facial reconstruction are both very important to forensics. Both have a unique role when investigating a crime. Facial recognition is used to try to positively identify a suspect. This can be done through an eyewitness or if there is a picture technology can be used .
What is facial reconstruction and what is it used for?
Facial reconstruction is a method used in the forensic field when a crime involves unidentified remains. Facial reconstruction is usually performed by a sculptor who is an expert in facial anatomy.
9Cancer is defined as the uncontrollable growth of cells that invade and cause damage to surrounding tissue. Oral cancer appears as a growth or sore in the mouth that does not go away. Oral cancer, which includes cancers of the lips, tongue, cheeks, floor of the mouth, hard and soft palate, sinuses, and pharynx (throat), can be life threatening if not diagnosed and treated early.
What Are the Symptoms of Oral Cancer?
 The most common symptoms of oral cancer include:
The most common symptoms of oral cancer include:
Swellings/thickenings, lumps or bumps, rough spots/crusts/or eroded areas on the lips, gums, or other areas inside the mouth
The development of velvety white, red, or speckled (white and red) patches in the mouth
Unexplained bleeding in the mouth
Unexplained numbness, loss of feeling, or pain/tenderness in any area of the face, mouth, or neck
Persistent sores on the face, neck, or mouth that bleed easily and do not heal within 2 weeks
A soreness or feeling that something is caught in the back of the throat
Difficulty chewing or swallowing, speaking, or moving the jaw or tongue
Hoarseness, chronic sore throat, or change in voice
Ear pain
A change in the way your teeth or dentures fit together
Dramatic weight loss
What do the early stages of mouth cancer look like?
In the early stages, mouth cancer rarely causes any pain. Abnormal cell growth usually appears as flat patches. A canker sore looks like an ulcer, usually with a depression in the center. The middle of the canker sore may appear white, gray, or yellow, and the edges are red.
Is oral cancer is curable?
If oral cancer is discovered early, the cure rate is nearly 90%. If, however, the cancer has already spread before diagnosis, the survival rate is 60% after five years of treatment. The best outcome for oral cancer is always early diagnosis and treatment.
What is the main cause of oral cancer?
Using tobacco plus alcohol poses a much greater risk than using either substance alone. HPV. Infection with the sexually transmitted human papillomavirus (specifically the HPV 16 type) has been linked to a subset of oral cancers. ...Cancer of the lip can be caused by sun exposure.