|
|
| Male Erectile Dysfunction : |
| |
 INTRODUCTION : INTRODUCTION :
In recent years, the importance of physical factors in the aetiopathogenesis of male erectile dysfunction has become incontrovertibly established. It is now known that erectile dysfunction can occur as a result of psychological factors, physical factors or both.
HISTORY-TAKING
Too often, history-taking is performed very cursorily; this can lead to great blunders. Because of the intimate admixture of psychological and physical issues in erectile function, a detailed psychosexual, marital and social history is mandatory. Such a history not only improves the diagnostic yield but also goes a long way in planning proper treatment. Importantly, it can help avert many a post-operative disaster should the candidate require surgery.
A detailed sexual history is invaluable. Direct questions should be asked about the rigidity and duration of erections during sleep, masturbation and sexual intercourse. History-taking should also include a systematic check list for contributory organic factors (Table 1). Often, a good history alone can lead the clinician to a working diagnosis of the relative preponderance of psychological or physical factors in any given patient.
PHYSICAL EXAMINATION
Although physical examination often contributes very little to the eventual diagnosis and treatment plan, the importance of its thoroughness cannot be over¬emphasized. A thorough general and local examination must be performed. A complete neurological examination is especially important because the diagnosis of neurogenic impotence is still made mainly by elimination of other causes coupled with a high index of clinical suspicion.
 INVESTIGATIONS INVESTIGATIONS
a) General
Systemic investigations contribute little to the diagnosis and management of impotence per se. However, these must be performed in the interest of the general health of the patient and to identify contributory underlying causes. Monitoring of diabetes, for example, does little to alter the continuing impact of the diabetic process on the erectile apparatus. The same is perhaps true for other systemic diseases associated with erectile dysfunction. It must be noted that even endocrine disorders usually affect the libido rather than the erection itself. Hormonal measurements, therefore, do not obviate the need for more specific tests.
b) Specific
The armamentarium of diagnostic gizmos and devices flooding the impotence market is quite confusing to the newcomer dabbling in impotence. While some of these are indubitably useful, many are mere research tools that contribute little to an objective diagnosis. Besides, the international literature on the subject is very contradictory and clear standards have not been enunciated for many of these tests. |
| |
| |
| A HISTORY |
| ■ |
Genitourinary disease |
| ■ |
Vascular or endocrine disease |
| ■ |
Systemic debilitating disease |
| ■ |
Neurologic disease |
| ■ |
Surgery - vascular, neurologic, |
| |
spinal, inguinal, pelvic |
| ■ |
Trauma - genital, pelvic, spinal |
| ■ |
Sleep disorders |
| ■ |
Psychologic history |
| ■ |
Marital and sexual history |
| ■ |
Erections-nocturnal, early |
| |
morning, non-incoital |
| ■ |
Medication |
| ■ |
Tobacco or alcohol use |
| ■ |
Other drug abuse |
| |
|
|
|
| |
B RISK FACTORS
- Diabetes mellitus
- High blood pressure
- Family history of 1) or 2)
- Medication for high B.P.
- Other medication (see D)
- Obesity
- Chronic smoking
- Excessive alcohol
- Sedentary life and lack of exercise
+ any of above
- Any condition listed in (A)
|
|
|
C COMMON ORGANIC CAUSES |
| Diabetes mellitus |
33% |
| Vascular disease |
25% |
| (e.g. high B P) |
|
| Pelvic surgery |
10% |
| Trauma (incl.spinal) |
08% |
| Endocrine disease |
06% |
| Medicines |
08% |
| Drug abuse |
07% |
| Multiple sclerosis |
03% |
|
|
| |
D) DRUGS CAUSING IMPOTENCE
Legal-tobacco, alcohol lllegal-cannabis, LSD, cocaine Iatrogenic
Endocrine
oestrogens
anti-androgens
LHRH analogues
5a reductase inhibitors
Anti-hypertensives
diuretics
methyldopa
ß blockers
Ca antagonists
Psychotropics
major tranquilisers
MAO inhibitors
tricyclic anti-depressants
Others
histamine-receptor antagonists
anti-hyperlipidaemics |
|
|
|
|
| |
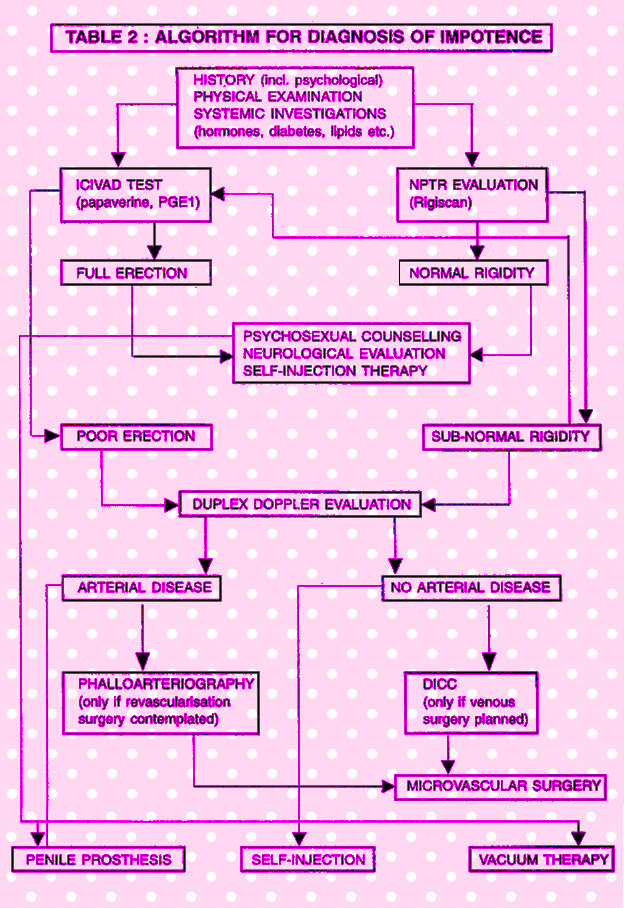
 It is still possible, however,- with the modalities available today to make a fairly accurate diagnosis of the predominant causal factor/s in any patient. It is not necessary to perform all tests on all patients. The work-up should be tailored according to the individual needs of the patient. Apart from the patient's economic capacities, time is an important consideration especially in case of the patients coming from faraway places. The psychological make-up and the attitude of the patient are also important. An invasive test should be eschewed in favour of non-invasive ones in especially anxious. The ultimate goal of the investigative work-up is to determine whether the cause of the impotence is psychological, arterial, venous, neurological or endocrinological. It is important to remember that often many factors may co-exist in the same patient. It is still possible, however,- with the modalities available today to make a fairly accurate diagnosis of the predominant causal factor/s in any patient. It is not necessary to perform all tests on all patients. The work-up should be tailored according to the individual needs of the patient. Apart from the patient's economic capacities, time is an important consideration especially in case of the patients coming from faraway places. The psychological make-up and the attitude of the patient are also important. An invasive test should be eschewed in favour of non-invasive ones in especially anxious. The ultimate goal of the investigative work-up is to determine whether the cause of the impotence is psychological, arterial, venous, neurological or endocrinological. It is important to remember that often many factors may co-exist in the same patient.
1) The Injection Test
If performed correctly, this test alone can enable a working diagnosis within one day. Drugs used are prostaglandin or papaverine hydrochloride. Prostaglandin is preferable when the patient has to travel within a few hours because of the much lesser risk of priapism. Many other vaso-active substances and their combinations (most notably papaverine - phentolamine) have been described. However, these are not indispensable and their non¬availability should not be a deterrent to an accurate diagnosis. Papaverine hydrochloride alone is adequate for most purposes. It is cheap and freely available throughout India. Prolonged erections and priapism, should they occur, are very easy to treat. The biggest enemy of papaverine is the anxious patient. For these reasons, it is very important that the patient's anxiety should be allayed. If necessary, the test should be repeated on more than one occasion.
 If there is no suspicion of neurological disease, it is safe to start with a dose of 45-60 mg. A 26-30 gauge needle is used to inject the drug directly into the corpora cavernosa at the mid-shaft level. The patient should always be given the privacy of a quiet, relaxed room. This test should never be performed in a busy out-patient setting with people walking in and out. This is certain to affect the outcome of the test. If there is no suspicion of neurological disease, it is safe to start with a dose of 45-60 mg. A 26-30 gauge needle is used to inject the drug directly into the corpora cavernosa at the mid-shaft level. The patient should always be given the privacy of a quiet, relaxed room. This test should never be performed in a busy out-patient setting with people walking in and out. This is certain to affect the outcome of the test.
The patient should be seated upright during the injection. Pressure on the puncture site should be very gentle or it can have a retrograde milking effect on the penis. This can lead to false-negative results even after appropriate dosage and can cause drug-related systemic side effects as well.
After injection, the penis should be gently stroked in order to distribute the drug and facilitate the lubricating jelly help. Visual Sexual Stimulation (VSS) using erotic literature, computer software or video films may be used but doesn't always help. Unlike in the west, erotica does not have the same effect on the Indian male. This is probably because of socio-cultural and attitudinal differences.
Lastly, it must be remembered that erotic literature and films are prohibited by law in India. For these reasons, VSS can be safely omitted without notable compromise in diagnostic yield.
Likewise, it may or may not be very helpful to keep the patient in his sexual partner's company during the conduct of this test. Many men are embarrassed in their partner's presence and this might affect the outcome of the test.
 The patient remains seated throughout the test, it is best to seat the patient on a large bed with his back propped against a back-rest or a wall. The legs should be stretched out on the bed. These simple precautions will prevent , accidental injuries which could arise from the systemic effects of papaverine hydrochloride. The patient remains seated throughout the test, it is best to seat the patient on a large bed with his back propped against a back-rest or a wall. The legs should be stretched out on the bed. These simple precautions will prevent , accidental injuries which could arise from the systemic effects of papaverine hydrochloride.
If the patient is relaxed and a suitable dose has been injected, a good erection will occur within 10 minutes. Erectile dysfunction secondary to arterial disease may take several minutes longer to produce an erection.
Patients with neurogenic impotence may develop priapism with very low doses of papaverine but this should not be a deterrent to using adequate dosages. If the erection is unequivocally rigid and the penis cannot be buckled, vasculogenic impotence can be virtually eliminated and no further investigations are necessary.
If the erection is not rigid enough, a second dose may be employed at the same sitting. This is quite safe and systemic side effects are uncommon.
However, it must be emphasised that this should be performed in a hospital setting with full infrastructural back-up rather than in an office environment. Any curvature of the penis can be studied at the same time.
If the erection is still not rigid enough, vascular disease must be eliminated using more sophisticated tests. A Doppler study can be easily combined with the injection test. If an objective measurement of the erection is desired either for academic, medico-legal or psychotherapeutic purposes, a real-time Rigiscan monitoring may be", performed at the same session.
All patients MUST be monitored to, for the next several hours until the erection has subsided completely. Haematomas and swellings are extremely rare if a very fine needle is used and adequate pressure is applied on the puncture site. No erection must be allowed to last longer than 4 to 6 hours. Blood-letting, performed using an 18 or 19 gauge scalp vein set should decompress nearly all erections. Vasoconstrictor antidotes and shunt operations are almost never necessary.
 2) The Rigiscan Test 2) The Rigiscan Test
The Rigiscan is the gold standard for NPTR (Nocturnal Penile Tumescence and Rigidity) measurement. It is the test of choice for non-invasive diagnosis.
It is especially suitable for anxious patients since it can be performed in the privacy of their own bedrooms. Its ability to objectively quantify erectile rigidity and establish physical normalcy makes it an important, reassurance-providing device to the patient with purely functional problems. It is also useful in medico-legal cases. Time and cost are two relative deterrents.
A Rigiscan tracing showing a good number of erectile episodes with rigidity levels of 80% or more and a duration of 20 minutes or more in a single episode almost effectively rules out serious vascular disease.
Arterial insufficiency and venous leaks can also be suspected on the basis of the Rigiscan graphs. Patients with purely arterial disease generally have low levels of maximum rigidity but of adequate duration.
Patients with predominant venous leakage will have varying rigidity levels depending on the severity of the leakage but the duration is almost always shortened. These patients must be evaluated using other means. The erectile response to vaso-active injection can be objectively studied by the concomitant application of the Rigiscan monitor. This is called a Realtime study.
 3) Penile Ultrasound 3) Penile Ultrasound
A Doppler evaluation of the penile arteries is indicated if the «rectile response to the injection test is inadequate or if the patient's Rigiscan study is suggestive of arterial insufficiency. Pure arterial disease is relatively uncommon in the young patient unless there is congenital arterial dysplasia, premature arterial disease or trauma.
Ultrasonographic evaluation of the cavemosal arteries can be performed with varying degrees of sophistication once cavemosal smooth muscle has been effectively relaxed by vaso-active injection. A simple acoustic Doppler probe, which is inexpensive and portable, emits auditory signals which can effectively eliminate gross cavernosa! arterial disease. Duplex Doppler and Colour Doppler studies can help visualisation of the cavemosal arteries and
measurement of flow.
They can also hint at the presence of venous disease. But while these are useful for quantifying penile arterial flow and help diagnose abnormalities in the main cavernosal arteries, they cannot altogether eliminate arterial insufficiency because of their inability to image the microvasculature. Thus, a normal arterial study does not eliminate arterial disease. This is important to bear in mind.
4) DICC (Dynamic Infusion Cavernosometry & Cavernosography)
The DICC is an useful haemodynamic test for the diagnosis of CVOD (Corporal Veno-Occlusive Dysfunction). In its simplest form, two cannulae are inserted into the corpora cavernosa after smooth muscle relaxation has been achieved with a vaso-active injection. One cannula is connected to a pressure transducer; the other conducts saline or radio-opaque contrast solution at controlled flow rates through an adjustable flow pump. Pressures are measured after injection and 30 seconds after a pressure of 150 mm Hg has been induced. Flow rates are measured in order to induce erection and attain ISO mm Hg, to maintain erection at 150 mm Hg, and to maintain mean arterial pressure  (MAP) - generally 80-90 mm Hg. The study is then repeated at a pressure setting of 90 mm Hg. The Cavernosal Artery Systolic Occlusion Pressure (CASOP) is also measured at the sametime using a Doppler device. These are also the only universally accepted standards for DICC evaluation. There are some centres that perform an 8 or 9 track multi-phasic DICC. Radiologic visualisation of leaking penile veins (cavernosography) is performed at the same sitting in many centres. Such radiologic studies are useful only if site-specific, selective ligation is planned as a surgical option. (MAP) - generally 80-90 mm Hg. The study is then repeated at a pressure setting of 90 mm Hg. The Cavernosal Artery Systolic Occlusion Pressure (CASOP) is also measured at the sametime using a Doppler device. These are also the only universally accepted standards for DICC evaluation. There are some centres that perform an 8 or 9 track multi-phasic DICC. Radiologic visualisation of leaking penile veins (cavernosography) is performed at the same sitting in many centres. Such radiologic studies are useful only if site-specific, selective ligation is planned as a surgical option.
5) Neurologic Evaluation
Many tests have been used for the evaluation of neurogenic impotence. These include nerve conduction studies, biothesiometry and corpus cavernosum electromyography (CCEMG), among others. None of these is 100% reliable. The diagnosis of neurogenic impotence continues to be based on elimination of vasculogenic causes, a high index of clinical suspicion and a thorough neurological examination. In any case, tests for neurogenic impotence, whatever their results, will not alter treatment" options. |
| |
 |
 Drug Induced Sextual Dysfunction Drug Induced Sextual Dysfunction
Side effects of drugs are not an uncommon occurrence and may occur frequently or infrequently in association with a drug or group of drugs, may or may not be* dose related, may be tolerable or unacceptable, may be related to pathophysiological effects of the drug or may be idiosyncratic. Sexual side effects of drugs occur probably more frequently than are reported in the literature, partly because physicians do not elicit the symptoms and patients are reluctant to mention them. They are more common with antihypertensive agents and psychotropic drugs but may occur with almost any drug - legal (alcohol), illegal (cocaine, marijuana) or prescribed. Sexual side effects occur probably equally in males and females but are reported more frequently in males because it is relatively easy to elicit history of erectile or ejaculatory dysfunction in men than to elicit history of sexual experience in women. It is also difficult to separate out components of sexual dysfunction related to physical effects of underlying disease process and psychological effects of illness and from the drug effect and it is equally possible that sexual dysfunction may have antedated either the development of illness or the drug therapy.
Sexual dysfunction may manifest itself in a number of different ways and they are shown in Table 1 |
| |
Table 1. TYPES OF SEXUAL DYSFUNCTION |
| 1. |
Sexual Desire Disorders |
| |
Decreased or loss of libido |
| |
Increased Kbido |
| 2. |
Erectile Disorders |
| |
Impotence |
| |
Priapism |
| 3. |
Ejaculatory Disorders |
| |
No or delayed ejaculation |
| |
Retrograde ejaculation |
| |
Painful ejaculation |
| |
Spontaneous ejaculation |
| 4. |
Delayed or no orgasm |
| 5. |
Decreased vaginal lubrication |
|
|
| |
 SEXUAL DESIRE DISORDERS SEXUAL DESIRE DISORDERS
Libido is characterised by a hormonally derived biological need for sexual activity and has an underlying neurochemical substrate in the limbic system of the brain. It is positively influenced by psychological events or by various sources of sexual stimuli. Medial preoptic area on the ventral diencephalon functions as a sexual drive control centre and neurons within this area receive synaptic terminals from peptidergic, dopaminergic, adrenergic and serotonergic neurons and contains receptors for reproductive hormones.
Drug induced sexual desire disorders may be due to alteration in patient's general mood or activity or by an effect on the activity within the pathways that specifically regulate the expression of sexual behaviour. In addition, drugs can have selective effects on sexual behaviour through the effects on brain areas that are responsible for regulating sexual drive by affecting various neurotransmitters or their actions. Drugs can also affect libido by affecting the hormonal milieu.
LOSS OF LIBIDO
Many drugs have been reported to cause loss of sexual desire. |
| |
Table 2 : DRUGS CAUSING LOSS OF LIBIDO |
| ■ |
Antihypertensive Drugs |
| |
Methyldopa |
| |
Clonidine |
| |
Beta Blockers |
| |
Indapamide |
| |
Guanethidine |
| |
Gurandrel |
| ■ |
Antidepressants |
| |
Desipramine |
| |
Nortriptyline |
| |
Amitriptyiine |
| ■ |
Hormonal Agents |
| |
Oestrogens (in men) |
| |
Progesterone |
| |
Danazol |
| ■ |
Miscellaneous |
| |
Benzodiazepines |
| |
Cimetidine |
| |
Narcotic analgesics |
|
|
| |
 Drugs that depress general behaviour or activity include hypnotics, sedatives, minor tranquilizers and major tranquilizers with sedative side effects cause 5l|eereased sexual desire. Drugs that depress general behaviour or activity include hypnotics, sedatives, minor tranquilizers and major tranquilizers with sedative side effects cause 5l|eereased sexual desire.
Nonselective beta blockers like propranolol cross tine blood brain barrier and inhibit central brain receptor, producing sedation or depression which may lead to loss of libido.
Drugs can cause loss of libido by altering the secretion or effects of reproductive hormones. Drugs tKat decrease dopaminergic receptor activity e.g. antipsychotic agents or catecholamine depleting drugs, suppress sexual function by induction of hyperprolactinaemia and secondary hypogonadism. Drugs with antiandrogen activity such as cyproterone acetate, flutamide, finasteride and cimetidine also decrease libido. Spironolactone suppresses synthesis of androgens and causes tegs of libido.
 INCREASED LIBIDO INCREASED LIBIDO
A variety of drugs have been reported to increase libido. The mechanisms of drug action in increasing sexual drive are diverse; the antidepressants may act primarily byVrelieving depression or they may share central catcholaminergic properties with other drugs causing hypersexual behaviour such as sympathomimetics, dopaminergic agents, amphetamines and cocaine. Hormones with sexual effects, like testosterone or anabolic steroids, may increase libido in men.
In laboratory animals, increased sexual behaviour can be induced by altering catecholamine metabolism through increasing synthesis with L-dopa, or decreasing degradation with a monoamine oxidase B inhibitor, deprenyl. Amphetamine, a catecholamine releasing agent and cocaine, a catecholamine uptake inhibitor increases sexual behaviour in rats and libido in men following acute administration.
The theory of dopaminergic receptor involvement is further supported by the observations of increased libido in patients being treated with dopamine agonist, e.g. apomorphine, pergolide and dopamine reuptake inhibitors, e.g. nomifensine and bupropion. 20-30% of patients with parkinsonism treated with levodopa report change in sexual activity including increased libido. Bromocriptine, a selective dopamine-2 agonist, may augment sexual behaviour in man. It is well established that hyperprolactinaemic states secondary to pituitary microadenomas, renal failure and other states are associated with diminished libido which is not alleviated by testosterone replacement but is reversed by bromocriptine therapy. Prolactin released by the pituitary lactotropin is under trophic inhibition by the catecholamine dopamine, therefore, the dopamine agonist bromocriptine will lower prolactin concentration and can restore gonadotropin secretion and gonadal function.
 Yohimbine, an alpha-2 adrenergic antagonist increases sexual behaviour by blocking presynaptic autoreceptors and increasing adrenergic receptor activity. Other alpha-2 adrenergic antagonists such as idazoxan, imiloxan and atizpepamezole are currently under preclinical and clinical studies on sexual response. Yohimbine, an alpha-2 adrenergic antagonist increases sexual behaviour by blocking presynaptic autoreceptors and increasing adrenergic receptor activity. Other alpha-2 adrenergic antagonists such as idazoxan, imiloxan and atizpepamezole are currently under preclinical and clinical studies on sexual response.
DISORDERS OF ERECTION
Men has two types of erection - reflexogenic and psychogenic.
Neuropharmacological agents affecting cholinergic, adrenergic, dopaminergic and serotonergic system affect erectile response both at central and peripheral levels.
 ERECTILE DYSFUNCTION ERECTILE DYSFUNCTION
Erectile dysfunction (ED) is defined as inability of the male to achieve erection of penis as part of the overall multi-affected response of the male sexual function. This definition takes away the emphasis on sexual intercourse as the sine qua non of sexual life and gives equal importance to other aspects of male sexual behaviour. Impotence, on the other hand, is defined as the inability of a man to achieve or maintain erection sufficient to permit satisfactory sexual intercourse. Impotence and ED are often used interchangeably in literature but the current acceptable terminology is ED rather than impotence.
A large number of drugs have been reported to cause ED. In general, majority of antihypertensive drugs, antidepressants, major tranquilizers and antiandrogens are major offenders and they act through different mechanisms.
|
Table 3: DRUGS CAUSING ERECTILE DYSFUNCTION |
| |
■ Antihypertensive Drugs
Centrally acting sympatholytics (e.g. clonidine, methyldopa) Peripherally acting sympatholytics (e.g. guandrel)
Beta Blockers
Thiazides
■ Antidepressants
MAO inhibitors
Tricyclic antidepressants
■ Antipsychotics
■ H2 Blockers (e.g. cimetidine)
■ Spironolactone
■ Ketoconazole
■ Miscellaneous
Antianxiety drugs (e.g. diazepam)
Sedatives (e.g. barbiturates)
Alcohol
Heroin |
| |
|
|
| |
 ANTIHYPERTENSIVE DRUGS ANTIHYPERTENSIVE DRUGS
Almost all available antihypertensive agents have been implicated in causiiif ED. The range of incidence of ED reported with various agents is so wide fls'tft be meaningless but some agents have been implicated more often than others.
DIURETICS
Thiazide diuretics, even though they have no direct CNS, autonomic or hormonal effects, have been associated with ED. Zinc depletion induced changes m hormonal milieu may be responsible.
Spironolactone induces ED by its antiandrogenic properties. It inhibits binding of dihydrotestosterone to androgen receptors which results in increased clearance of testosterone and increased conversion of testosterone to oestradiol. Larger doses of spironolactone block 17-hydroxylase, an enzyme necessary in the biosynthesis of steroids. This blockade of 17-hydroxylase results in decreased serum testosterone levels.
 BETA BLOCKERS BETA BLOCKERS
Beta blockers primarily affect erectile function by decreased beta-2 mediated vasodilation and unopposed alpha-1 vasoconstriction of the corpora cavernosum. Beta blockers with decreased lipid solubility (like atenolol) with less ability to penetrate blood brain barrier or beta-1 selective beta blockers may have reduced incidence of ED. Labetalol, a combined alpha and beta blocker also does not often cause ED
.
CENTRAL ADRENERGIC AGONIST - SYMPATHOLYTICS
Methyldopa functions as a central alpha adrenergic agonist and also a false neurotransmitter which inhibits sympathetic outflow. It also increases prolactin levels. AH these mechanisms lead to ED in a large number of patients. Clonidine stimulates presynaptic alpha adrenergic receptors which decreases sympathetic outflow and this is responsible for ED.
NEWER DRUGS
Angiotensin converting enzyme inhibitors, calcium channel blockers, direct vasodilators like minoxidil have rarely been implicated in causing ED and should be considered for use in patients with hypertension with preexistent ED or who develop ED while being treated with one of the above agents.
 PSYCHOTROPIC DRUGS PSYCHOTROPIC DRUGS
ED caused by psychotropic agents is frequently related to their anticholinergic properties. Thioridazine which has strong anticholinergic properties is twice as likely to cause ED compared to nonthioridazine antipsychotic agent like haloperidol. Some of the antipsychotic agents also cause hyperprolactinaemia due to their --»-dopamine blocking properties. Thioridazine, again, has greater adrenergic inhibitory effect and leads to greater effects on hypothalamic-pituitary-gonadal axis than other antipsychotic agents and results in higher levels of prolactin and greater suppression of testosterone.
DRUG INDUCED PRIAPISM
Priapism is defined as pathological, painful and prolonged erection of the penis, generally unrelated to sexual stimulation, excitation or sexual activity and that involves corpora cavernosa, while the corpus spongiosum and the glans penis remain flaccid.
Priapism most often results from obstruction of venous outflow from the corpora cavernosa of the penis and this may be due to physical obstruction of the venous drainage as may occur in patients with sickle cell disease or leukaemia or due to functional obstruction of the venous outflow as may occur with changes in the sympathetic/parasympathetic tone which may occur with medications. A number of drugs have been reported to cause priapism and they are listed in Table 4.
|
| Table 4: DRUGS CAUSING PRIAPISM |
| PSYCHOTROPIC DRUGS |
ANTIHYPERTENSIVE DRUGS |
MISCELLANEOUS |
| Antidepressants |
Prazosin |
Papaverine |
| Trazodone |
Hydralazine |
Heparin |
| Phelelzine |
Labetalol |
Bromocriptine |
| Antipsychotics |
Phenoxybenzamine |
Tamoxifen |
| Chlorpromazine |
Nifedipine |
Testosterone |
| Thioridazine |
|
Phenytoin |
| Fluphenazine |
|
Buspirone |
| Thiothixene |
|
Pergolide |
| Haloperidol |
|
Gecaine |
| Mesoridazine |
|
Molindone |
| Clozapine |
|
Fat emulsion |
|
| |
 Role of adrenergic nervous system in erectile function is supported by studies that show that direct penile injection of alpha-adrenergic antagonists can result in penile erection and this can be reversed by injection of alpha agonist. Normally there is a balance between cholinergic and adrenergic nervous system that determines tumescence and deturnescence. If there is increased parasympathetic tone in relation to sympathetic tone, priapism may result due to failure of deturnescence. Role of adrenergic nervous system in erectile function is supported by studies that show that direct penile injection of alpha-adrenergic antagonists can result in penile erection and this can be reversed by injection of alpha agonist. Normally there is a balance between cholinergic and adrenergic nervous system that determines tumescence and deturnescence. If there is increased parasympathetic tone in relation to sympathetic tone, priapism may result due to failure of deturnescence.
Most psychotropic agents have anticholinergic effects and hence priapism is not a common side effect of psychotropic medications. However priapism may occur if patients are sensitive to alpha adrenergic blocking effects of these drugs. Trazodone possesses strong alpha-1 blocking properties while lacking direct anticholinergic properties and is the drug most frequently implicated in causing priapism. Ability of other psychotropic agents like chlorpromazine and thioridazine is also mediated by alpha blockade. Prazosin also is an alpha blocker and priapism can be induced by this drug by a similar mechanism. Labetalol is a combined alpha and beta blocker and its alpha blocking properties result in priapism.
Most cases of priapism are due to venous outflow obstruction but occasional cases are due to abnormal increase in arterial flow and vasodilators like hydralazine; papaverine may induce priapism by such a mechanism. Delay in treatment may lead to thickening and oedema of corpora cavernosa and result in impotence. In addition to stopping the offending drug, the treatment of drug induced priapism, as for all cases, is to remove the stagnant blood from corpora cavernosa. In the early phases, aspiration of corpora cavernosa and irrigation with saline may be all that is needed but priapism of long duration requires that a shunt procedure be carried out. Medications that havebeen used to reverse priapism include alpha adrenergic compounds like phenylephrine, ephedrine, norepinephrine  injected in corpora cavernosum after penile aspiration. injected in corpora cavernosum after penile aspiration.
EJACULATORY DISORDERS
During the ejaculatory phase of sexual response, there are rhythmic contractions of epididymis, vas deferens, seminal vesicles and prostate which expel seminal fluid into the prostatic urethra. As the urethral bulb is stimulated, reflex closure of the bladder neck prevents retrograde ejaculation. Rhythmic contractions of the urethral bulb and striated perineal musculature then propel the seminal fluid.
forward in the process of ejaculation. As in the case of behavioural and erectile phases, dopaminergic and sertotonergic modulate the central component of ejaculatory reflex while alpha adrenergic stimulation is implicated in seminal emission and bladder neck closure. Role of cholinergic nervous system in the process of ejaculation is not clear.
NO OR DELAYED EJACULATION
Agents that decrease dopaminergic activity increase ejaculatory latency and reduce ejaculatory capacity. One of the postulated mechanisms of ejaculatory failure caused by antipsychotic agents may be the central effects of these agents in decreasing dopaminergic activity.
 A number of commonly prescribed antidepressants including imipramine, amitriptyline and isocarboxazid are associated with ejaculatory failure. These agents block the reuptake of 5-HT and increase serotonin levels. Sertraline and fluoxetine are selective 5-HT uptake inhibitors and produce delayed ejaculation. Interestingly these effects of antidepressants (both tricyclic and MAO inhibitors) can be reversed by administration of cyproheptadine, a drug with antiserotonergic properties. A number of commonly prescribed antidepressants including imipramine, amitriptyline and isocarboxazid are associated with ejaculatory failure. These agents block the reuptake of 5-HT and increase serotonin levels. Sertraline and fluoxetine are selective 5-HT uptake inhibitors and produce delayed ejaculation. Interestingly these effects of antidepressants (both tricyclic and MAO inhibitors) can be reversed by administration of cyproheptadine, a drug with antiserotonergic properties.
Pharmacological agents that deplete functional pools of catecholamines or have alpha-1 adrenergic antagonist activity predictably impair emission, ejaculation, and the experience of orgasm. The agents that diminish presynaptic norepinephrine release include reserpine, methyldopa, guanethidine. Agents with significant alpha-1 adrenergic antagonist activity include antihypertensive agents like phenoxybenzamine, phentolamine, prazosin, labetalol, psychotropic agents like chlorpromazine, thioridazine, trifluoperazine, phenelzine, amitriptyline and clomipramine.
RETROGRADE EJACULATION
During the process of ejaculation, there is reflex closure of the internal urethral sphincter which prevents retrograde ejaculation and this is mediated predominantly by alpha-1 adrenergic nervous system.
 Drags that possess alpha-1 adrenergic antagonist properties can cause retrograde ejaculation and these agents include all the drugs mentioned in the previous section. Sympathomimetic agents such as pseudoephedrine, ephedrine, and phenylpropanolamine have been used to treat retrograde ejaculation. Drags that possess alpha-1 adrenergic antagonist properties can cause retrograde ejaculation and these agents include all the drugs mentioned in the previous section. Sympathomimetic agents such as pseudoephedrine, ephedrine, and phenylpropanolamine have been used to treat retrograde ejaculation.
MISCELLANEOUS EJACULATORY DISORDERS
Spontaneous ejaculation has been described to occur in patients being treated with trifluoperazine, thiothixene and mazindol and pergolide, while painful ejaculation has been reported in patients being treated with clomipramine, haloperidol, imipramine, protriptyline, thioridazine and trifluoperazine.
DISORDERS OF ORGASM
Orgasm in man consists of a pleasurable sensation associated with emission and ejaculation but orgasm can occur independent of ejaculation. It results from cerebral processing of afferent stimuli from the dorsal and pudendal nerves. Orgasm in women consists of a pleasurable sensation that usually begins at the clitoris and rapidly spreads throughout the pelvis and is marked by simultaneous rhythmic muscular contractions of the uterus, outer third of vagina and the anal sphincter.
D isorders of orgasm can occur both in men and women but are frequently described in literature in women. isorders of orgasm can occur both in men and women but are frequently described in literature in women.
Psychotropic drugs have often been associated with anorgasmia (inability to have orgasm) and the offending agents include selective serotonin reuptake inhibitors (SSRI) like fluoxetine, paraxetine and sertraline, MAO inhibitors like phenelzine, isocarboxazid and tranylcypromine, tricyclic antidepressants like clomipramine and major tranquilizer like thioridazine.
Common strategies to overcome this drug side effect include waiting for tolerance to develop, dose reduction, change of dosing regimen, partial drug holiday , substitution of alternative antidepressant (bupropion, an aminiketone has no negative sexual side effects and actually has been reported to significantly increase libido, level of arousal, intensity of orgasm beyond levels experienced premorbidly), coadministration of another drug (e.g. mianserin, cyproheptadine, low doses of psychostimulants like methyphenidate or dextroamphetamine added toSSRIs). |
|
| |
|







