Dr. Prasenjit Kr. Roy
IVF Surgeon in Siliguri & Malda, India
MBBS, MS (G&O)
Fellowship in Reproductive Endocrinology & Infertility
(Tel-Aviv University, Israel)
Call Doctor +91 98832 01323
MBBS, MS (G&O)
Fellowship in Reproductive Endocrinology & Infertility
(Tel-Aviv University, Israel)
Call Doctor +91 98832 01323
IVF, otherwise known as In Vitro Fertilisation, is a method of getting pregnant where an egg is fertilised by sperm outside of the body, in vitro (which means in glass). The resulting embryos can then be transferred to the woman's uterus with the intention of establishing a successful pregnancy. The process is undertaken by couples struggling to conceive, same-sex couples or single women wishing to have a baby through sperm donation.

IVF is for:
Women aged under 40 years who have not conceived after 2 years of regular unprotected intercourse.
Women suffering from endometriosis
Couples with a genetic condition which can be screened for in the embryo
Women with premature ovarian failure
Women with blocked or damaged fallopian tubes
Women with ovulatory disorders
Women with polycystic ovarian syndrome
Patients for whom treatments such as artificial insemination have failed
Same-sex couples and single women
Male factor infertility, including decreased sperm count or sperm motilityWomen with ovulation disorders, premature ovarian failure, uterine fibroids
Women who have had their fallopian tubes removed
Individuals with a genetic disorder
Unexplained infertility.
Intrauterine insemination (IUI) is one of the most straightforward forms of assisted fertility treatments, the goal of which is to increase the number of sperm that reach and fertilise the egg on their own. It involves placing sperm inside a woman's uterus to facilitate fertilisation. This form of fertility treatment is a less invasive and less expensive option in comparison to in vitro fertilisation.
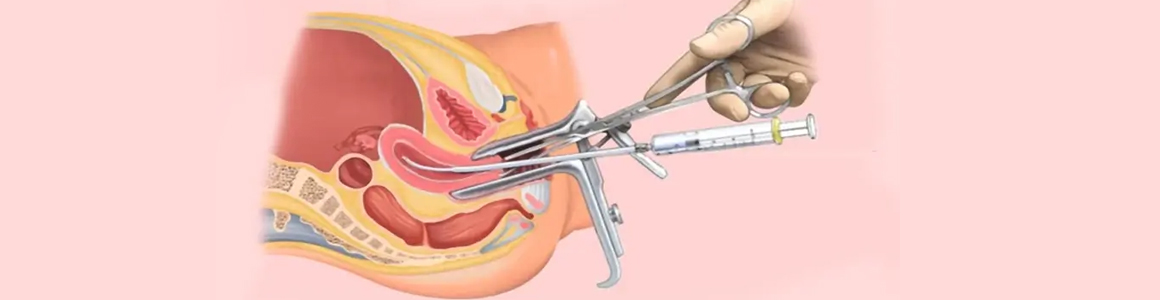
When is IUI Used
IUI is most commonly used when a partner has a low sperm count or decreased sperm motility. However, it can also be the preferred fertility treatment for any of the following conditions:
Couples whose reasons for subfertility are unknown.
Ejaculation dysfunction.
A hostile cervical condition, including cervical mucus difficulties.
Cervical scar tissue from past procedures which may hinder the sperms' ability to enter the uterus.
Ovulations complications.
Abnormality of the cervix.
Couples with reduced sperm count or motility
ICSI is very similar to conventional IVF in that gametes (eggs and sperm) are collected from each partner. The difference between the two procedures is the method of achieving fertilisation.
In conventional IVF, the eggs and sperm are mixed together in a dish and the sperm fertilises the egg 'naturally'. However to have a chance that this will occur, large numbers of actively swimming normal sperm are required. For many couples, the number of suitable sperm available may be very limited or there may be other factors preventing fertilisation, so conventional IVF is not an option. ICSI has provided a hope for these couples.
ICSI refers to the laboratory procedure where a single sperm is picked up with a fine glass needle and is injected directly into each egg. This is carried out in the laboratory by experienced embryologists using specialist equipment. Very few sperm are required and the ability of the sperm to penetrate the egg is no longer important as this has been assisted by the ICSI technique. ICSI does not guarantee that fertilisation will occur as the normal cellular events of fertilisation still need to occur once the sperm has been placed in the egg.
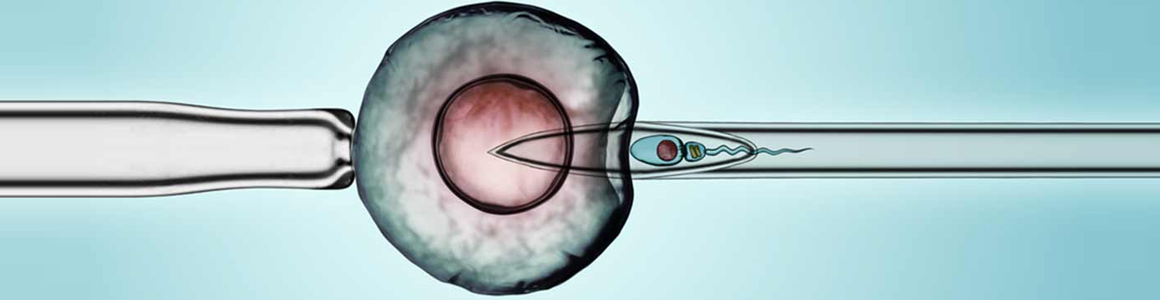
Who is ICSI suitable for -
From a patient perspective, undergoing an ICSI treatment cycle is exactly the same as a conventional IVF cycle, and the same steps are involved.
When the sperm count is very low
When the sperm cannot move properly or are in other ways abnormal
When sperm has been retrieved surgically from the epididymis (MESA/PESA) or the testes
(TESE/TESA), from urine or following electro-ejaculation
When there are high levels of antibodies in the semen
When there has been a previous fertilisation failure using conventional IVF.
The usual way of producing sperm for use in Assisted Reproductive Technology is manual stimulation. In cases where medical or religious factors prevent this, surgical methods can be used. Medical reasons that could contribute to inability to produce sperm though ejaculation could consist of azoospermia, low sperm count, low sperm motility. The following procedures help retrieve sperm through minor surgical procedures:
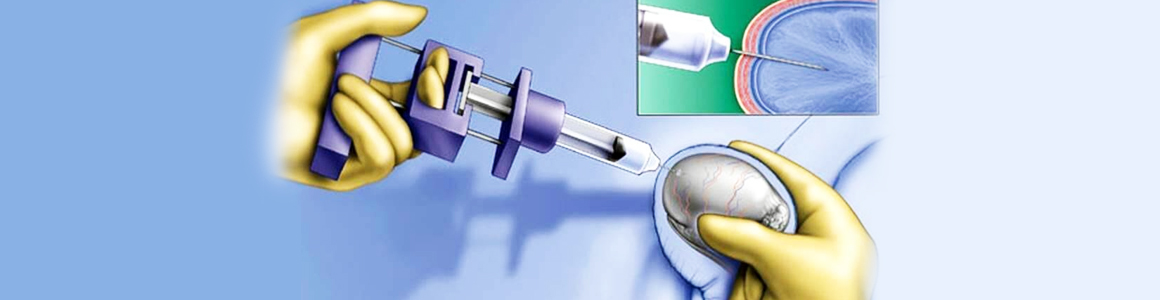
PESA
PESA (percutaneous epididymal sperm aspiration) is a method, performed under local anesthesia, which involves extracting sperm with a fine needle from the epididymis or testes. The sperm is then implanted into the egg through the process of ICSI (Intracytoplasmic Sperm Injection) to be used in IVF.
TESA & TESE
In cases where the epididymis does not contain any sperm, because of impaired sperm production, the method of TESA (Testicular Sperm Aspiration) or TESE (Testicular Sperm Extraction) may be used. TESE involves a surgical biopsy of the testis, while TESA is performed by sticking a needle into the testis and aspirating fluid and tissue with negative pressure.
MESA
The most invasive of the surgical sperm retrieval procedures is MESA (micro-epididymal sperm aspiration), which is performed under general anesthesia. MESA involves the cutting open of the scrotum to retrieve sperm. The wound is closed with dissolvable stitches. Swelling and pain subsides within a few days, during which prescribed painkillers may be taken to ease the pain.
These alternative methods of retrieving sperm allow male patients to use their own sperm in the IVF procedure. The procedures themselves are not very costly and offer the chance for couples to avoid the cost of using a sperm donor. At the Cyprus Fertility Clinic, we are committed to offering you low cost IVF treatment with high success rates.
Some men do not produce sperm at all or only in insufficient numbers and poor quality. Many of these men can have their sperm aspirated directly from their testicles (TESA) or from the epididymis that stores the sperm prior to an ejaculation (PESA, MESA).
The retrieved sperm are then used during in vitro fertilization, gestational surrogacy or egg donation treatments with Intracytoplasmic Sperm Injection (ICSI).
Egg donation forms part of a method of assisted reproduction. It has become increasingly common in recent years due to the social tendency for women to postpone having children until later on in life, when their fertility is often reduced. This method of assisted reproduction is also useful in many other situations and circumstances - for women with ovarian failure, hereditary diseases, chromosomal abnormalities, or those affected by endometriosis, to name just a few examples. Egg donation makes the most of our modern-day knowledge and understanding of biology, genetics, fertility and technology, in order to enable women and couples who may be struggling or unable to conceive a child to fulfil that wish. The process involves a donor giving her eggs to a recipient patient, who has requested them so to increase her chances of becoming pregnant and having her own biological child.
Why someone might opt for egg donation :
A patient may choose to opt for egg donation as a form of assisted reproduction for various reasons. These range from primary or premature ovarian failure to the failure of a fertility treatment like In Vitro Fertilisation (IVF), or from a natural reduction of fertility as women get older to specific diseases such as endometriosis. In fact, although egg donation plays a large role in helping women over the age of 40 to become pregnant, a quarter of The IVI Group's patients are affected by endometriosis. And it is for that reason that we are pioneering research into this chronic disease, to increase awareness and understanding of its causes and symptoms. Endometriosis causes growth of endometrial tissue outside the uterus, and it can lead to a decline in a woman's pool and quality of oocytes (therefore, her fertility and chances of conception). However, what is important here is that this diagnosis can be mitigated or alleviated, thanks to innovative assisted reproduction methods such as egg donation.
Surrogacy is a method of assisted reproduction that helps intended parents (IPs) start families when they otherwise could not. Intended parents pursue surrogacy for several reasons and come from different backgrounds. All intended parents work with a gestational surrogate, a woman who carries a child to term.
There are two types of surrogacy arrangements: gestational surrogacy and traditional surrogacy. Circle Surrogacy only provides gestational surrogacy arrangements, which means the gestational carrier has no genetic connection to the child. Through in vitro fertilization (IVF), embryos are created in a lab (sometimes with the use of an egg donor) and are transferred into the surrogate mother's uterus. In a traditional surrogacy arrangement, a surrogate becomes pregnant with the use of her own eggs.

Who Needs a Surrogate Mother:
Medical Reasons for Surrogacy
One of the most common reasons a couple might choose to consider surrogacy is medically related. Some women have reproductive illnesses that prevent them from becoming pregnant, while others can become pregnant but can't carry full term. Women who have had illnesses that required a hysterectomy may look towards surrogacy as well.
Alternately, some couples look toward surrogacy not necessarily for reproductive reasons but to protect the health of the intended mother. Some women take medications that are life sustaining but that may harm a fetus. Stopping a medication for a pregnancy is not always a healthy or safe option.
Age Related Considerations
According to reproductivefacts.org, your chance of becoming pregnant declines with age. A 30-year old woman in good health has a 20% chance of becoming pregnant each month. A 40-year old woman has a 5% chance. A later-in-life decision to start a family may not be impossible, but it may not be healthy for a woman to carry a fetus full-term.
Same-Sex Couples
Couples in same-sex relationships can't start families without some sort of help. Women may look towards sperm donation so that one mother can carry the baby full-term, but two men will always need the help of either the surrogate or adoption process.
Recurrent pregnancy loss is classically defined as the occurrence of three or more consecutive pregnancy loss; however, the American Society of Reproductive Medicine (ASRM) has recently redefined recurrent pregnancy loss as two or more pregnancy losses. A pregnancy loss is defined as a clinically-recognized pregnancy involuntarily ending before 20 weeks. A clinically-recognized pregnancy means that the pregnancy has been visualized on an ultrasound or that pregnancy tissue was identified after a pregnancy loss.

What Causes Recurrent Pregnancy Loss:
Most pregnancy losses result from chromosomal, or genetic, abnormalities, and are random events. The abnormality may come from the egg, the sperm, or the early embryo. Approximately 12-15% of all clinically recognized pregnancies end in miscarriage; however, it is estimated that at least 30-60% of all conceptions will end within the first 12 weeks of gestation. Up to 50% of the time, the woman doesn't even realize that she was ever pregnant. The risk of miscarriage increases with the number of previous pregnancy losses, but is typically less than 50%.
Advancing maternal age is associated with an increased risk of miscarriage, which is thought to be due to poor egg quality leading to chromosomal (genetic) abnormalities. Sometimes, the mother or father themselves may have a slight irregularity in their genes, but the offspring could be more severely affected and thus result in miscarriage.
Sometimes, there could be an abnormality in the uterus (the womb) that leads to miscarriage. The miscarriage may be due to poor blood supply to the pregnancy or inflammation. Some women may be born with an irregularly shaped uterus, and some women may develop abnormalities with their uterus over time.
A woman's immune system may also play a role in recurrent pregnancy loss. Hormone abnormalities may also impact pregnancy loss, including thyroid disease and diabetes. Abnormalities in a mother's blood clotting may also affect pregnancy loss.
Generally speaking, environmental factors, stress, and occupational factors do not seem to be related to pregnancy loss
Recurrent pregnancy loss is classically defined as the occurrence of three or more consecutive pregnancy loss; however, the American Society of Reproductive Medicine (ASRM) has recently redefined recurrent pregnancy loss as two or more pregnancy losses. A pregnancy loss is defined as a clinically-recognized pregnancy involuntarily ending before 20 weeks. A clinically-recognized pregnancy means that the pregnancy has been visualized on an ultrasound or that pregnancy tissue was identified after a pregnancy loss.

What are the common causes of Male Infertility -
The root cause of a man's infertility may not be easy to establish. For up to 50% of men diagnosed with male factor infertility, the specific cause remains unknown. Generally, male fertility problems have to do with the quantity or quality of the sperm, though there can also be issues with ejaculation. While the reasons for these problems are often unclear, most of the treatment options remain the same whatever the underlying cause may be. Some of the more common causes include:
Pre-existing genetic conditions
Hormone disorders
Injury to the groin area
Previous surgeries, such as hernia repair or vasectomy
Previous infections, especially STDs, urinary tract infections or a severe mumps infection after puberty.
Exposure to poisonous chemicals or radiation (most common in cancer survivors.)
There are also certain lifestyle choices which may impact a man's fertility, such as wearing tight or restrictive underwear or using tobacco, alcohol, or other drugs.