Since its introduction in the late 1980s, laparoscopic cholecystectomy has become the treatment of choice for symptomatic gallstone disease. Today more than 75% of cholecystectomies are performed laparoscopically. By choosing laparoscopic cholecystectomy vs. open cholecystectomy , the patient can achieve a better cosmetic result with less scarring, a faster recovery with return to normal activity and a shorter hospital stay. Regretfully, there are a variety of laparoscopic cholecystectomy complications. These complications include bowel perforation, infection, hemorrhage and burns, but for the purposes of this article we will concentrate on the most serious complication: bile duct injury. The incidence of bile duct injury during laparoscopic cholecystectomy has decreased but remains as high as 1.4%. During this discussion I hope to offer an overview of the pertinent anatomy, a description of the surgical procedure and a discussion of the complications and most common surgical repairs.
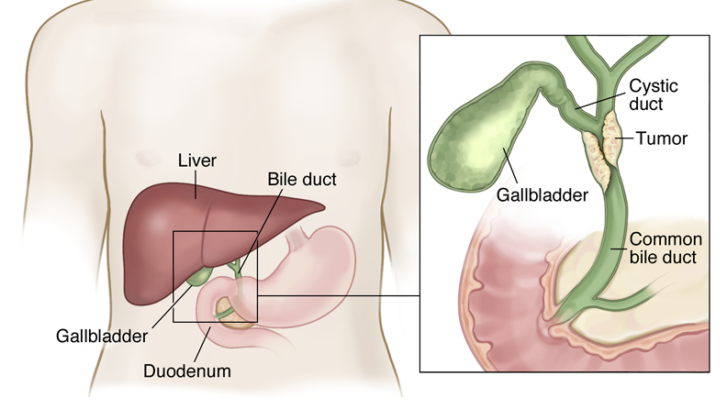
The gallbladder is a pear-shaped sac that is attached to the bottom surface of the liver. It stores bile between meals, concentrates the bile by reabsorbing water and releases the bile when needed to help the body digest fatty foods. Bile is carried from the liver and gallbladder to the small intestine via the bile ducts. The largest of these ducts is the common bile duct. This duct is formed by a joining of the common hepatic duct that leads down from the liver and the cystic duct that leads from the gallbladder. The common bile duct is vitally important since it is the only pathway through which bile can travel from the liver to the intestines.
A laparoscopic cholecystectomy is the surgical removal of the gallbladder that does not require a large open abdominal incision. Several small openings are created with sharp instruments called trocars. A laparoscope and other surgical instruments are inserted through these openings and controlled via a view through the scope. The scope is often assisted by a small video camera mounted in the scope. The procedure is relatively straightforward. The cystic duct and cystic artery leading to the gallbladder must be clipped and divided, the gallbladder dissected free from the liver and then the gallbladder can be removed. But it is vitally important that the surgeon properly identify the cystic duct prior to the clipping or division of the bile duct. Mistakes in the identification of the bile ducts can often lead to injury to the common hepatic duct or common bile duct. These injuries include excision, division, narrowing and occlusion of these structures.
Narrowing or occlusion of the bile ducts can lead to a back up of bile leading to damage to the liver. Excision or division of the bile ducts results in leakage of bile into the abdominal cavity leading to widespread infection and peritonitis. This can damage multiple organs and even result in fatal sepsis. Complications are generally minimal if the errors are realized during surgery or recognized promptly. The most serious cases generally involve delays or failure to diagnose the complications. Treatment of intra-operative bile duct injuries often involves a complex open procedure called a hepaticojejunostomy (or Roux-en-Y) in which a loop of small intestine is divided and pulled up to the liver where the small bowel is connected directly with the damaged bile duct. This procedure is much more involved than the original laparoscopic cholecystectomy procedure and results in all of the post-operative negatives that the laparoscopic technique had attempted to avoid. These negatives include pain, scarring, extended hospital stay and prolonged recovery. In worse cases, continued complications can result in multiple surgeries, progressive deterioration and even death. Even in the best cases, patients experiencing iatrogenic bile duct injuries will experience a decreased quality of life moving forward.