A liver abscess occurs when bacteria or protozoa destroy hepatic tissue, producing a cavity, which fills with infectious organisms, liquelled liver cells, and leukocytes. Necrotic tissue then walls off the cavity from the rest of the liver. Liver abscess occurs equally in men and women, usually in those over age 50. Death occurs in 15% of affected patients despite treatment.
Underlying causes of liver abscess include benign or malignant biliary obstruction along with cholangitis, extrahepatic abdominal sepsis, and trauma or surgery to the right upper quadrant. Liver abscesses also occur from intra-arterial chemoembolizations or cryosurgery in the liver, which causes necrosis of tumor cells and potential infection.
The method by which bacteria reach the liver reflects the underlying causes. Biliary tract disease is the most common cause of liver abscess. Liver abscess after intra-abdominal sepsis (such as with diverticulitis) is most likely to be caused by hematogenous spread through the portal bloodstream. Hematogenous spread by hepatic arterial flow may occur in infectious endocarditis.
Abscesses arising from hematogenous transmission are usually caused by a single pathogen; those arising from biliary obstruction are usually caused by a mixed flora. Patients with metastatic cancer to the liver, diabetes mellitus, and alcoholism are more likely to develop a liver abscess.
The organisms that predominate in liver abscess are gram-negative aerobic bacilli, enterococci, streptococci. and anaerobes. Amebic liver abscesses arc caused by E. histolytica.
The clinical manifestations of a liver abscess depend on the degree of involvement. Some patients are acutely ill; in others, the abscess is recognized only at autopsy, after death from another illness.
The onset of symptoms of a pyogenic abscess is usually sudden; in an amebic abscess, the onset is more insidious. Common signs include abdominal pain, weight loss, fever, chills, diaphoresis, nausea, vomiting, and anemia. Signs of right pleural effusion, such as dyspnea and pleural pain, develop if the abscess extends through the diaphragm. Liver damage may cause jaundice.
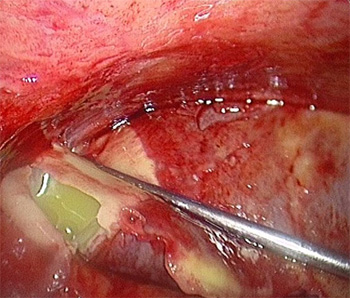
Ultrasonography and computed tomography (CT) scan with contrast medium can accurately define intrahepatic lesions and allow assessment of intra-abdominal pathology. Percutaneous needle aspiration of the abscess can also be performed with diagnostic tests to identify the causative organism. Contrast-aided magnetic resonance imaging may become an accurate method for diagnosing hepatic abscesses.
Abnormal laboratory values include: elevated levels of serum aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, and bilirubin; an increased white blood cell count; and decreased serum albumin levels. In pyogenic abscess, a blood culture can identify the bacterial agent; in amebic abscess, a stool culture and serologic and hemagglutination tests can isolate E. histolytica.
Antibiotic therapy, along with drainage, is the preferred treatment for most hepatic abscesses. Pereutaneous drainage, either with ultrasound or CT guidance, is usually sufficient to evacuate pus. Surgery may be performed to drain pus in unstable patients with continued sepsis (despite attempted non surgical treatment) and for patients with persistent fevers (lasting longer than 2 weeks) after percutaneous drainage and appropriate antibiotic therapy. A common combination is ampicillin, an amino glycoside, and either metronidazole or clindamycin. Third-generation cephalosporins can be substituted for the aminoglycosides in patients at risk for renal toxicity. When the causative organisms are identified, the antibiotic regimen should be modified to match the patient's sensitivities. I.V. antibiotics should be administered for 14 days and then replaced with oral preparations to complete a 6week course. Surgery is reserved for bowel perforation and rupture into the pericardium.
1. Provide supportive care, monitor vital signs (especially temperature), and maintain fluid and nutritional intake.
2. Administer anti-infective's and antibiotics as necessary, and watch for possible adverse effects. Stress the importance of compliance with therapy.
3. Explain diagnostic and surgical procedures.
4. Watch carefully for complications of abdominal surgery, such as hemorrhage or sepsis.
5. Prepare the patient for I.V antibiotic administration as an outpatient with home care support.