Dr. Sankar Dasmahapatra
High Risk Pregnancy Doctor in Kolkata, India
DGO, MS, Fellowship in Gynaecological Lap Surgery (Sydney -Australia)
Consultant Gynaecologist & Obstetrician
Infertility Specialist & Lapaoscopic Surgeon
DGO, MS, Fellowship in Gynaecological Lap Surgery (Sydney -Australia)
Consultant Gynaecologist & Obstetrician
Infertility Specialist & Lapaoscopic Surgeon
SOME UNIQUE SUCCESS STORIES
Mother Deliver Premature Twins at The Age of 44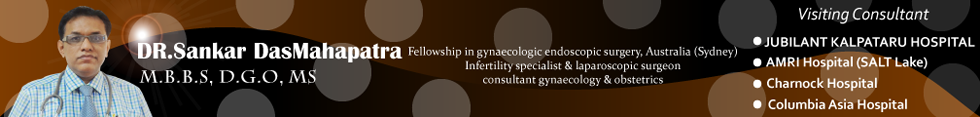
Dr.Sankar DasMahapatra performs best cesarean section surgery in Kolkata. Providing cesarean section or C section Surgery in Kolkata over last 20 years at very affordable cost. Dr.Mahapatra has performed hundreds of successful cesarean delivery in Kolkata. Dr.Sankar Das MahaPatra is attached with best hospitals in Kolkata conducting cesarean section or C section delivery.”
What is a cesarean section?
A cesarean section, also called a c-section, is a surgical procedure performed when a vaginal delivery is not possible or safe, or when the health of the mother or the baby is at risk. During this procedure, the baby is delivered through surgical incisions made in the abdomen and the uterus.
When would I need a cesarean section?
A cesarean delivery might be planned advance if a medical reason calls for it, or it might be unplanned and take place during your labor if certain problems arise.
You might need to have a planned cesarean delivery if any of the following conditions exist:
• Cephalopelvic disproportion (CPD) — CPD is a term that means that the baby’s head or body is too large to pass safely through the mother’s pelvis, or the mother’s pelvis is too small to deliver a normal-sized baby.
• Previous cesarean birth — Although it is possible to have a vaginal birth after a previous cesarean, it is not an option for all women. Factors that can affect whether a cesarean is needed include the type of uterine incision used in the previous cesarean and the risk of rupturing the uterus with a vaginal birth.
• Multiple pregnancy — Although twins can often be delivered vaginally, two or more babies might require a cesarean delivery.
• Placenta previa — In this condition, the placenta is attached too low in the uterine wall and blocks the baby’s exit through the cervix.
• Transverse lie — The baby is in a horizontal, or sideways, position in the uterus. In this condition, a cesarean delivery is always used.
• Breech presentation — In a breech presentation, or breech birth, the baby is positioned to deliver feet or bottom first. If the baby cannot be turned through abdominal manipulation, Gynaecologist proccedes for cesarean delivery.
An unplanned cesarean delivery might be needed if any of the following conditions arise during your labor:
• Failure of labor to progress — In this condition, the cervix begins to dilate and stops before the woman is fully dilated, or the baby stops moving down the birth canal.
• Cord compression — The umbilical cord is looped around the baby’s neck or body, or caught between the baby’s head and the mother’s pelvis.
• Prolapsed cord — The umbilical cord comes out of the cervix before the baby does.
• Abruptio placentae — The placenta separates from the wall of the uterus before the baby is born.
• Fetal distress — During labor, the baby might begin to develop problems that cause an irregular heart rate. Gynaecologist Dr.Sankar Das Mahapatra might decide that the baby can no longer tolerate labor and that a cesarean delivery is necessary.

Most of the time having a baby is a natural process. After a full-term pregnancy, a woman goes into labor on or near her due date and gives birth to a healthy baby. A day or two later she leaves the hospital to begin day-to-day life with her growing family. But not all pregnancies go smoothly. Some women experience what doctors refer to as a high-risk pregnancy.
A pregnancy is considered high-risk when there are potential complications that could affect the mother, the baby, or both. High-risk pregnancies require management by a specialist to help ensure the best outcome for the mother and baby.
Risk Factors for High-Risk Pregnancy
Reasons that a pregnancy may be considered high risk include:
1) Maternal Age: One of the most common risk factors for a high-risk pregnancy is the age of the mother-to-be. Women who will be under 17 or over 35 when their baby is due are at greater risk of complications than those between their late teens and early 30s. The risk of miscarriage and genetic defects further increases after age 40.
2) Medical conditions that exist before pregnancy: Conditions such as high blood pressure; breathing, kidney, or heart problems; diabetes; autoimmune disease; sexually transmitted diseases (STDs); or chronic infections such as human immunodeficiency virus (HIV) can present risks for the mother and/or her unborn baby. A history of miscarriage, problems with a previous pregnancy or pregnancies, or a family history of genetic disorders are also risk factors for a high-risk pregnancy.
If you have a medical condition, it's important to consult your doctor before you decide to become pregnant. Your doctor may run tests, adjust medications, or advise you of precautions you need to take to optimize the health of you and your baby.
3) High-risk pregnancy: Know what to expect
A high-risk pregnancy can be stressful. Know what kind of prenatal care you might need and how to cope.
A high-risk pregnancy might pose challenges before, during or after delivery. If you have a high-risk pregnancy, you and your baby might need special monitoring or care throughout your pregnancy. Understand what causes a high-risk pregnancy, and what you can do to take care of yourself and your baby.
What are the risk factors for a high-risk pregnancy?
Sometimes a high-risk pregnancy is the result of a medical condition present before pregnancy. In other cases, a medical condition that develops during pregnancy for either mom or baby causes a pregnancy to become high risk.
Specific factors that might contribute to a high-risk pregnancy include:
• Advanced maternal age. Pregnancy risks are higher for mothers age 35 and older.
• Lifestyle choices. Smoking cigarettes, drinking alcohol and using illegal drugs can put a pregnancy at risk.
• Medical history. A prior C-section, low birth weight baby or preterm birth — birth before 37 weeks of pregnancy — might increase the risks for subsequent pregnancies. Other risk factors include a fetal genetic condition, a family history of genetic conditions, a history of pregnancy loss or the death of a baby shortly after birth.
• Underlying conditions. Chronic conditions — such as diabetes, high blood pressure and epilepsy — increase pregnancy risks. A blood condition, such as anemia, an infection or an underlying mental health condition also can increase pregnancy risks.
• Pregnancy complications. Various complications that develop during pregnancy pose risks, such as problems with the uterus, cervix or placenta, or severe morning sickness (hyperemesis gravidarum) that continues past the first trimester. Other concerns might include too much amniotic fluid (polyhydramnios) or too little amniotic fluid (oligohydramnios), restricted fetal growth or Rh (rhesus) sensitization — a potentially serious condition that can occur when your blood group is Rh negative and your baby's blood group is Rh positive.
• Multiple pregnancy. Pregnancy risks are higher for women carrying twins or higher order multiples.
• Overdue pregnancy. You might face additional risks if your pregnancy continues too long beyond the due date.

What steps can I take to promote a healthy pregnancy?
Whether you know ahead of time that you'll have a high-risk pregnancy or you simply want to do whatever you can to prevent a high-risk pregnancy, stick to the basics. For example:
• Schedule a preconception appointment. If you're thinking about becoming pregnant, consult your health care provider. He or she might counsel you to start taking a daily prenatal vitamin and reach a healthy weight before you become pregnant. If you have a medical condition, your treatment might need to be adjusted to prepare for pregnancy. Your health care provider might also discuss your risk of having a baby who has a genetic condition.
• Be cautious when using assisted reproductive technology (ART).If you're planning to use ART to get pregnant, consider how many embryos will be implanted. Multiple pregnancies carry a higher risk of preterm labor.
• Seek regular prenatal care. Prenatal visits can help your health care provider monitor your health and your baby's health. Depending on the circumstances, you might be referred to a specialist in maternal-fetal medicine, genetics, pediatrics or other areas.
• Eat a healthy diet. During pregnancy, you'll need more folic acid, calcium, iron and other essential nutrients. A daily prenatal vitamin can help fill any gaps. Consult your health care provider if you have special nutrition needs due to a health condition, such as diabetes.
• Gain weight wisely. Gaining the right amount of weight can support your baby's health — and make it easier to shed the extra pounds after delivery. A weight gain of 25 to 35 pounds (about 11 to 16 kilograms) is often recommended for women who have a healthy weight before pregnancy. If you're overweight before you conceive, you might need to gain less weight. If you're carrying twins or triplets, you might need to gain more weight. Work with your health care provider to determine what's right for you.
• Avoid risky substances. If you smoke, quit. Alcohol and illegal drugs are off-limits, too. Get your health care provider's OK before you start — or stop — taking any medications or supplements.

Do I need special tests?
If you have a high-risk pregnancy, you might consider various tests or procedures in addition to routine prenatal screening tests. Depending on the circumstances, your health care provider might recommend:
• Specialized or targeted ultrasound. This type of fetal ultrasound — an imaging technique that uses high-frequency sound waves to produce images of a baby in the uterus — targets a suspected problem, such as abnormal development.
• Amniocentesis. During this procedure, a sample of the fluid that surrounds and protects a baby during pregnancy (amniotic fluid) is withdrawn from the uterus. Typically done after week 15 of pregnancy, amniocentesis can identify certain genetic conditions, as well as neural tube defects — serious abnormalities of the brain or spinal cord.
• Chorionic villus sampling (CVS). During this procedure, a sample of cells is removed from the placenta. Typically done between weeks 10 and 12 of pregnancy, CVS can identify certain genetic conditions.
• Cordocentesis. This test, also known as percutaneous umbilical blood sampling, is a highly specialized prenatal test in which a fetal blood sample is removed from the umbilical cord. Typically done after week 18 of pregnancy, the test can identify chromosomal conditions, blood disorders and infections.
• Cervical length measurement. Your health care provider might use an ultrasound to measure the length of your cervix at prenatal appointments to determine if you're at risk of preterm labor.
• Lab tests. Your health care provider might take a swab of your vaginal secretions to check for fetal fibronectin — a substance that acts like a glue between the fetal sac and the lining of the uterus. The presence of fetal
fibronectin might be a sign of preterm labor.
• Biophysical profile. This prenatal test is used to check on a baby's well-being.
The test combines fetal heart rate monitoring (nonstress test) and fetal ultrasound.
