Dr. Sankar Dasmahapatra
Gynecologists and Obstetricians in Kolkata, India
DGO, MS, Fellowship in Gynaecological Lap Surgery (Sydney -Australia)
Consultant Gynaecologist & Obstetrician
Infertility Specialist & Lapaoscopic Surgeon
DGO, MS, Fellowship in Gynaecological Lap Surgery (Sydney -Australia)
Consultant Gynaecologist & Obstetrician
Infertility Specialist & Lapaoscopic Surgeon
Dr. Sankar Dasmahapatra is personally familiar with many of the concerns and issues women and couples face. His years of clinical experience, both in the india and abroad, have deepened his understanding further and have also allowed him insight into other cultures and customs. He fervently believes that each one of his patients is an individual with individual circumstances and treatment needs, and these he aims to address with a sympathetic ear and an open mind in his practice.

Dr. Sankar Dasmahapatra :: Consultant Gynaecologist and Obstetrician provides consultations on :
Preconception counseling is an appointment with your healthcare provider that’s used to plan for a future pregnancy. Your family history, risk factors, medical conditions and lifestyle are all discussed. This appointment is an important part of a planned and healthy pregnancy.
What is preconception counseling?
Having a safe, healthy and happy pregnancy begins well before you have a positive result on a test. Caring for your health before you become pregnant helps you prepare for a pregnancy. Preconception counseling is a visit with your healthcare provider where you discuss many aspects of pregnancy and plan for a healthy pregnancy.

When should I schedule a preconception counseling appointment?
This appointment should happen at least three months before you start trying to get pregnant.
What will my provider discuss with me during a preconception counseling appointment?
During the visit, your healthcare provider will discuss the following topics:
A) Family history: Your family history—and your partner’s family history—can provide insight about any genetic conditions or disorders that may be passed on to a child. Understanding your medical past can help your healthcare providers treat you and your child in the future. This information may also tell your healthcare provider if they need to perform extra tests or watch for the development of certain conditions during pregnancy. Specific parts of your family health history to share with your doctor could include a history of :
- Hypertension (high blood pressure).
- Diabetes.
- Mental disorders.
- Blindness.
- Deafness.
- Birth defects (congenital conditions).
- Ethnicity-related diseases (Tay-Sachs, sickle trait/sickle cell disease).
- Twins or multiples.
B) Your general medical history: It is important for your provider to see the whole picture of your health before pregnancy. During your appointment, your caregiver will want to discuss:
- Surgeries, hospitalizations or transfusions you may have had in the past.
- Any pre-existing medical conditions.
- Any allergies.
- Any medications you may currently be taking.
C) Your OB/GYN history: During the discussion of your medical history, your doctor will ask you about your OB/GYN history. Some STIs and vaginal infections can affect a woman’s ability to conceive. Your doctor may do cervical cultures or blood tests to make sure there are no infections that could cause issues during conception or pregnancy. Specific topics your provider may discuss include:
- Any previous pregnancies.
- Your menstrual history.
- Contraceptive use.
- Any sexually transmitted infections (STIs).
- Any history of known uterine abnormalities.
- Pap smears or any treatments for abnormal paps.
- Vaginal infections.
D) Lifestyle: A healthy lifestyle is very important during pregnancy. This includes a balanced and nutritious diet, exercise, and stopping any drug use and smoking, as well as exposure to any environmental hazards.
E) Vaccination: Your provider may need to update or give you additional vaccinations before you become pregnant. Some of these vaccinations may require time between when they are given to you and when you become pregnant. Bring your vaccination records with you to your appointment.

What happens during my preconception counseling appointment?
During preconception counseling, your provider may do several tests. These tests may include:
A physical exam: Your provider may do a physical exam during your preconception appointment. This exam may involve your caregiver:
- Checking your heart, lungs, breasts, thyroid, and abdomen.
- Doing a pelvic exam.
- Checking your blood pressure.
- Recording your weight.
Lab tests: These tests are used to check for various diseases and conditions. Lab tests may include:
- Testing for rubella.
- Testing for hepatitis.
- Complete blood count (CBC).
- A pap smear.
- Diabetes screening.
- Testing for thyroid issues.
- Testing for HIV.
Your provider may also discuss how to chart to your menstrual cycles and when you ovulate each month. You may be given a prenatal vitamin with 400 to 800 micrograms of folic acid. You should start taking this before you are pregnant. Your baby can benefit from a prenatal vitamin before you may even know you are pregnant.
What types of tests will my partner and I go through during preconception counseling?
Your doctor may suggest that both you and your partner go through genetic counseling before conceiving, especially if you have a family history of certain genetic conditions. This process will provide a lot of information to your healthcare team that could be helpful during your pregnancy. Genetic counseling can also pinpoint certain risk factors that your doctor will be able to discuss with you and plan for. You may also be tested for certain conditions like Tay-Sachs or sickle trait/sickle cell disease. These conditions can be passed down throughout families.

What happens after my preconception counseling appointment?
Your caregiver may make several suggestions after your appointment. These could be a mix of lifestyle changes and healthcare suggestions, including:
- Losing weight.
- Quitting smoking or drinking.
- Not taking medications that could be harmful to the pregnancy (always speak to your doctor before starting or stopping a medication).
- Updating your immunizations.
- Taking recommended vitamins (including prenatal vitamins).
- Avoiding extra stress.
- Seeing specialists for health problems before conceiving.
What other lifestyle changes should I keep in mind as I prepare for pregnancy?
During pregnancy, women can continue to exercise. Regular exercise (at least three times per week) is preferred over intermittent activity (altering between periods of being active and inactive). Pregnant women should stop exercising when fatigued and not exercise to exhaustion. It’s also very important to stay hydrated. Also, a good diet of healthy food is very important. Good nutrition during pregnancy is needed for your baby to grow and develop. During your pregnancy, you will need to consume about 300 more calories per day than you before pregnancy. Establishing a nutritious diet before you are pregnant can help you maintain good eating habits throughout all three trimesters.
Laparoscopic Endometriosis surgery treats mild to severe cases by skilled surgeons trained in this method. During the procedure, they'll make a small incision in your abdomen so they can insert a tiny tube with a camera (laparoscope) through it. In some cases, they may need to make more than one small incision.
Background
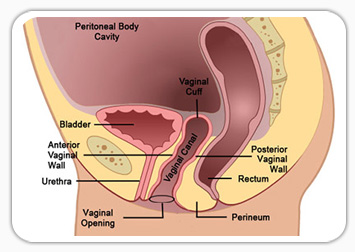
Girls with androgen insensitivity and vaginal agenesis are born without a functional vagina. There are several surgical methods available to create a neovagina including the McIndoe procedure which entails a skin graft, the Davydov procedure which utilizes peritoneal tissue, the Williams vulvovaginoplasty which uses vulvar tissue, and there is the option to create a vagina from a bowel graft. All these procedures are rather invasive with significant risk of scarring leading to failure of the procedure. The current literature supports dilation of a vaginal dimple as the overwhelmingly preferred method of creating a neovagina. Because of the natural elasticity of the tissues, a vagina can be created by self dilation in 3-6 months. This requires the patient, often a teenage girl, to diligently apply pressure with a dilator twice daily for twenty minutes for 3-6 months to achieve adequate vaginal length. Aside from being excessively time consuming; many girls are adverse to this method of treatment because they are both physically and psychologically uncomfortable with self treatment.

Complications and post-operative period
No intra- or post-operative complications were observed in any of the patients undergoing the surgical procedure. Post-operative recovery was rapid although post-operative need for analgetics was present in patients and ranged from 5 days to intermittent use of oral pain-relieving medication for up to 24 weeks (two of eight patients) with a median time of 11 weeks. Patients were discharged home between days 6 and 15 with a median post-operative stay of 13.8 days.
Conclusion
Taken together, the laparoscopic variant of the Vecchietti operation is a safe and effective method for creation of a neovagina in patients with MRKH. However, regular post-operative dilation of the reconstructed organ either by sexual intercourse or by use of dilators is necessary for satisfying long-term results of the procedure.
Cervical cancer is cancer that starts in the cells of the cervix. The cervix is the lower, narrow end of the uterus (womb). The cervix connects the uterus to the vagina (birth canal). Cervical cancer usually develops slowly over time.
What is the cause of cervical carcinoma?
Long-lasting infection with certain types of human papillomavirus (HPV) is the main cause of cervical cancer. HPV is a common virus that is passed from one person to another during sex.
What is the early symptom of cervical carcinoma?
Early-stage cervical cancer generally produces no signs or symptoms. Signs and symptoms of more-advanced cervical cancer include: Vaginal bleeding after intercourse, between periods or after menopause. Watery, bloody vaginal discharge that may be heavy and have a foul odor.
What is the survival rate of cervical carcinoma?
When cervical cancer is diagnosed at an early stage, the 5-year relative survival rate is 91%. When cervical cancer is diagnosed after it has spread to nearby tissues, organs, or regional lymph nodes, the 5-year relative survival rate is 60%.

What are the 5 warning signs of cervical cancer?
- Abnormal vaginal bleeding. Many women have the occasional irregular period or spotting, but changes that aren't typical for you could indicate something more serious....
- Unusual discharge....
- Painful sexual intercourse....
- Pain in the pelvic region....
- Complications in bowel movements.
What is the risk factor for cervical carcinoma?
Almost all cervical cancers are caused by HPV. Other things also can increase your risk of cervical cancer. Almost all cervical cancers are caused by human papillomavirus (HPV), a common virus that can be passed from one person to another during sex. There are many types of HPV.
What is the most common symptoms of patient with cervical carcinoma?
Cervical Cancer Symptoms
- vaginal bleeding after sex.
- vaginal bleeding after menopause.
- vaginal bleeding between periods or periods that are heavier or longer than normal.
- vaginal discharge that is watery and has a strong odor or that contains blood.
- pelvic pain or pain during sex.
Tingling, numbness and weakness in the arms, hands, legs or feet. Lack of coordination and difficulty walking. Loss of bladder or bowel control.
What is Stage 4 Cervical Carcinoma?(Cervical Cancer)
In stage IV, cervical cancer has spread beyond the pelvis, or has spread to the lining of the bladder or rectum, or has spread to other parts of the body. Stage IV is subdivided into stages IVA and IVB, based on where the cancer has spread.
Is cervical cancer painful?
Pain from cervical cancer may not feel like much in the early stages of the disease if you feel anything at all. As cancer progresses and spreads to nearby tissues and organs, you may experience pain in your pelvis or have issues urinating. Other people will feel generally unwell, tired or lose their appetite.
What is the first stage of cervical cancer?
Stage 1 means that your cancer is within the neck of the womb (cervix). It hasn't spread to nearby tissues or other organs.
How can I test for cervical cancer at home?
HPV Check is a comfortable and reliable at-home cervical cancer screening test that detects the Human papillomavirus (HPV), the virus that causes cervical cancer. HPV testing is now approved by the NHS as a reliable method of cervical cancer screening.
What is the recovery time for cervical surgery?
You may need to wear a neck brace for a while. Most people can go back to work after 4 to 6 weeks. But it may take a few months to get back to your usual activities. How long it takes depends on what kind of surgery you had and the type of work and other activities you do.
Irregular menstrual bleeding or heavy menstrual bleeding or a combination of both may characterize abnormal menstruation.
World wide up to 20% of women will suffer from heavy menstrual bleeding (HMB) at some point in their lives. It accounts for 12% of referral to gynaecology outpatient departments.
Historically up to 60% of women would end up with a hysterectomy within 5 years of referral but there are now a number of effective alternative ways to manage HMB without recourse to hysterectomy.
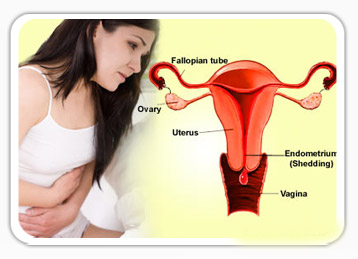
The holistic approach to the management of HMB is important as it depends on a woman’s symptoms as well as her circumstance, whether her family is complete or whether fertility is still desired. A woman should not be compelled to remove her womb if she doesn’t want to, and on the other hand she shouldn’t be forced to keep it if it is detrimental to her quality of life. This course of management is underpinned by NICE (National Institute of Clinical Excellence) guidelines in the UK.
In the absence of any overt pathology it is possible to manage HMB with medication in some cases hormones will not be required. The next step of management would then be hormonal manipulation. This may be in the form of tablets or the use of the Mirena™(a small device that is inserted in the womb and gives off low dose hormones) and if all this fails surgery may be required.
Even when surgery is required hysterectomy is not the starting point measures to remove or destroy the lining of the womb are effective treatments in up to 70% of women.
For women who do require hysterectomy tradition open surgery should not be and is no longer the norm. It is now possible to carry out most hysterectomies though minimal access techniques, sometimes irrespective of the size of the uterus.
The questions women should always ask her gynaecologist should always include: whether she is able to have her hysterectomy by minimal access techniques and if not why? Whether she needs to have her cervix removed during the hysterectomy and whether she needs to have her ovaries removed.
Cervical screening in the UK has been a success in screening to prevent cervical cancer, about 4.4 million women are screened in the UK each year. Screening starts at the age of 25 and goes on till 65 years provided the last smears have been normal.
No one knows what causes cervical cancer but there are associations with the human papilloma virus and cigarette smoking.
Recent advances in the screening and management process include screening for HPV types that have been linked with increased risk of developing cervical cancer and the use of Vaccines for prevention.
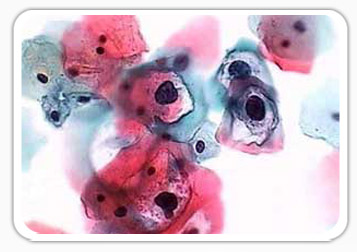
If abnormalities are found on screening they are usually graded as borderline, mild, moderate or severe.
Depending on circumstance it may be decided that colposcopy is required. This is an investigation where the neck of the womb ( the cervix) is examined under magnification (using an instrument akin to binoculars) to identify whether the abnormal cells found on the smear truly exist. If abnormality is found a biopsy may be taken and this will dictate whether further treatment is necessary. Sometimes treatment may be advised just on the basis of colposcopy.
Where treatment is required it is usually done by large loop excision of the transformation zone (LLETZ), with a local anaesthetic to numb the cervix.
The procedure takes about 10-15 minutes. Women are advised not to undertake vigorous exercise, have intercourse or use tampons for 3-4 weeks after the procedure. They are advised to return or make contact if they have bleeding that is heavier than a heavy period, as bleeding is a potential complication of the procedure. Long term complications are uncommon; they include cervical stenosis( where the cervix becomes too tight) or cervical incompetence (where the cervix is unable to stay closed during pregnancy) this may result in miscarriage. This complication is rare occurring in less than 0.5% of women.
Over 90% of women will need no further intervention after the first treatment for others however follow-up may be required.
Miscarriage presents with pain and or bleeding in early pregnancy, after missing a menstrual period. Unfortunately miscarriage is not uncommon. 1 in 8 pregnancies will miscarry. Once a woman has a positive pregnancy test within the first 3 months there is a 20% chance that she might miscarry. Between 6 and 9 weeks the risk falls to about 4% and after 9 weeks to 3% in the first trimester. The risk of miscarriage increases after a third miscarriage and with age.
From the early 1990s the management of miscarriage has changed in the United Kingdom with all units that care for women with complications of early pregnancy having dedicated areas and dedicated staff, who are experienced and versed in the management of complications of early pregnancy (Early pregnancy assessment units). These allow women continuity of care, provide counseling and support, and allow all tests and therapies to be carried out in dedicated areas, and avoid unnecessary and repeated internal examinations.
Once a woman experiences pain and bleeding in early pregnancy she will be referred to one of these units in her local area.

Miscarriages are usually defined as:
• Threatened: where there has been pain and or bleeding but the pregnancy is still ongoing.
• Inevitable Miscarriage: where there has been pain and bleeding but the neck of the womb (cervix) is open to such an extent that nothing can be done to stop the miscarriage from progressing to pregnancy loss
• Incomplete Miscarriage: where part of the pregnancy has already been lost and part remains in the womb
• Missed Miscarriage: where the baby has already died within the womb but remains inside the womb
On arrival at the EPAU the objective would be to try and determine what type of miscarriage is taking place. A pregnancy test is usually organised and depending on how many weeks pregnant the woman is an ultrasound scan is then arranged. If the fetal heart is seen beating on the ultrasound scan she is reassured and in most cases sent home. If any of the above types of miscarriages is identified management choices are:
• Expectant: where the pregnancy is given the chance to come out by itself without medical intervention
• Medical: where medication is given to encourage the failed pregnancy to come out of the womb without the need for surgery
• Surgical management
Traditionally surgical management was the only therapy offered but depending on a woman’s symptoms and her preference she may be offered expectant or medical management. There are certain criteria that need to be met for safety and efficacy of the first 2 methods of management.
Whatever management is offered women are offered counseling for the emotional implications of miscarriage and how if necessary to manage future pregnancy.
Endometriosis is a chronic condition where endometrium (this is the lining of the inside of the womb) is found outside the womb. It can be responsible for pelvic pain, pain during intercourse and in some women infertility.
It is common in the reproductive years but can also present in adolescence.
Unfortunately though it occurs in up to 10% of the general population with figures increasing in women with pelvic pain and infertility, Diagnosis is commonly delayed and women have often had numerous consultations before the eventual diagnosis is made
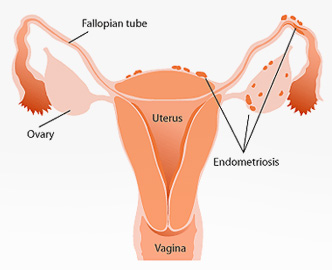
Though it is possible to diagnose some forms endometriosis with non- invasive techniques like ultrasound, the gold standard for diagnosis is a laparoscopy. This allows for the diagnosis to be made with certainty and the stage (severity) of the disease to be determined. It also allows the woman to make up her mind on how to manage her future fertility based on the information from the laparoscopy as fertility is known to decline after the age of 35 years and particularly so in women with endometriosis
The management of endometriosis requires a holistic and multidisciplinary approach as endometriosis not only affects the woman but may also affect indirectly other family members.
Management should be undertaken by experts who are not only familiar with the symptoms of the disease but also its natural history as endometriosis however treated has a recurrence risk and most women depending on the stage of endometriosis may require more than one surgery.
Initial management of endometriosis may be by the use of medicines or pain management therapy depending on the desire for immediate fertility. If fertility is not immediately desired then the pain symptoms can be managed with pain killers or in some cases the oral contraceptive pill.
Management multidisciplinary teams usually include a gynaecologist, a colorectal surgeon, urologists and pain management specialists as well as dedicated endometriosis nurses and support from counselors, physiotherapists and in some cases alternative medicine specialists. Women will only need to see certain specialists depending on their circumstance.
Women are also encouraged to join support groups to share experiences as in some cases a problem shared is a problem halved.
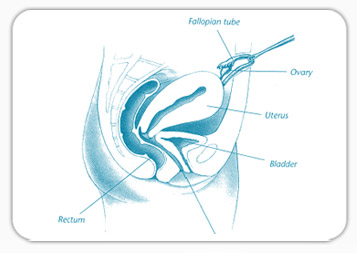
Ectopic pregnancy is a pregnancy that is situated outside the womb. The most common site is the fallopian tube. It is a potentially life-threatening condition and occurs in about 1:100 pregnancies.
Common symptoms are abdominal pain and bleeding after missing a menstrual period, with a positive pregnancy test.
Risk factors for ectopic pregnancy include: previous ectopic pregnancy, previous tubal surgery, previous pelvic infection, current IUCD use. Though most women who present with ectopic pregnancy will have none of these symptoms.
Ectopic pregnancies are usually diagnosed on the basis of symptoms and a blood test which measures the amount of Beta-HCG which is a pregnancy related hormone, and an ultrasound scan.
For the majority of women it is possible to make a diagnosis after initial investigation but in some women the results of investigations may be inconclusive and follow up scans and blood tests may be necessary.
Once the diagnosis is established women may be given a choice of how they would prefer their ectopic pregnancy to be managed. The choice is sometimes limited however by symptoms and the results of investigations.
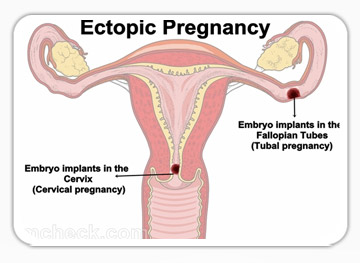
Choices include:
1) Conservative, Expectant management, where women are kept under surveillance until the pregnancy resolves by itself.
• Threatened: This management depends on the initial pregnancy hormone level when this is less than 1000IU, this meth
od of management is 70% successful.
2) Medical management: this is where a drug called Methotrexate is given to “kill” the rapidly dividing ectopic pregnancy cells. This modality of treatment depends on Beta-HCG levels and scan findings. The pregnancy may also take some time to resolve.
• For optimal chances of success the HCG level usually chosen is less than 3000IU, and there should be no fetal heart seen on ultrasound scan.
• Success is in the region of 88%.
• 15% of women may require a further injection.
• 7-10% of women may require surgical intervention.
3) Surgical management: the majority of women who have ectopic pregnancies are managed by surgery. Traditionally surgery used to be by conventional open surgery but now it is possible to manage nearly if not all ectopic pregnancies by means of laparoscopic surgery.
Despite evidence that laparoscopic surgery is superior to conventional surgery unfortunately not all women with this condition even if stable are managed by laparoscopic surgery with figures ranging from between 39% and 89% in india
Dr dasmahapatr has wide knowledge and research interest in this area. Under his direction all (100%) women who are haemodynamically stable have laparoscopic surgery for the management of ectopic pregnancy when this is required. Even in haemodynamically unstable women 85% are managed by means of laparoscopic surgery by a highly skilled team of surgeons, nurses and theatre.
Even for the rarer ectopic pregnancies Dasmahapatra has demonstrated that laparoscopic surgery is feasible.
Uterine fibroids are the commonest benign tumour (growth) of the female reproductive tract. Fibroids affects up to 30-40% of women. It is particularly common during the reproductive years and is more common in women of colour than Caucasians. Black woman tend to present with symptoms relating to fibroids earlier than Caucasians and they are more likely to present with problems relating to fertility.
No one knows for sure what causes fibroids but they develop from a single muscle cell in the uterus and are hormone dependent. They also tend to run in families.
Fibroids can be responsible for heavy periods leading to anaemia, pressure symptoms on the bowel where they may cause constipation. The effect on the bladder can either be going to the toilet to pass urine more often or in some cases they can cause retention of urine.
Fibroids can also be responsible for fertility problems depending on their location, particularly those within or distorting the cavity of the womb.
It must be said however that most women that have fibroids will have no problems with fertility and when they do get pregnant they will have no problems.
Some of the problems associated with fibroids in the pregnant women include: increased risk of miscarriage, increased risk of degeneration which may lead to pain, increased risk of premature delivery and increased risk of bleeding once the baby has been delivered.
The most important statement about the management of fibroids is “just because they are there does not mean they need to be removed” and that “the primary objective of management of fibroids is not to remove the fibroids but to do away with the symptoms they cause”.
To this end a woman who suffers with symptoms relating to the presence of fibroids needs to seek out a gynaecologist with experience in the management of all aspects of care relating to fibroids and not a gynaecologist who is an expert in only one aspect of management.
The objective of management should be to treat the symptoms, to facilitate or increase chances of fertility if this is what is desired, and while achieving these objectives ensure the best quality of life for the patient.
Treatment modalities for the management of fibroids include:
1. Medication:
• Non hormonal medication to reduce menstrual flow
• Hormonal preparations: these may reduce heavy menstrual loss and in some cases reduce the size of fibroids. Their effects are usually limited by side effects
2. The Mirena intrauterine contraceptive devic
3. Uterine artery embolization
4. Surgery
• Hysteroscopic transcervical resection of fibroids
• Myomectomy
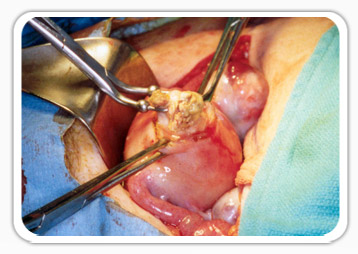
A) Laparoscopic myomectomy; this has the advantage of
(i) Reduced adhesion formation (scar tissue)
(ii) Less blood loss
(iii) Reduced pain
(iv) Reduced hospital stay
(v) Earlier return to normal activities
B) Traditional conventional surgery for removal of fibroids
Dr . Dasmahamahapatra of kolkata is familiar with all aspects of management of uterine fibroids and applies minimal access techniques where it is the responsible thing to do. Not all fibroids can or should be managed by minimal access means but where possible the size of the fibroid is not sole the limitation for minimal access management.
Though it is now possible to manage menstrual and other gynaecological pathologies conservatively some women will still be advised to have a hysterectomy.
Hysterectomy is one of the commonest major gynaecological operations performed with over 600,000 procedures performed in the USA.
For women who require hysterectomy the questions now asked are how should the hysterectomy be performed?
Despite the advantages of minimal access surgery for hysterectomy most women still undergo conventional surgery because of the expertise of their chosen surgeon.
NICE and other regulatory bodies advocate that the first choice for a hysterectomy should be vaginal, followed by laparoscopic and the last choice should be traditional open surgery.
Common reasons for open surgery include:
• The size of the uterus
• The need to remove ovaries at the same time
• No uterine descent particularly in women who have not had children
• Need to deal with another pathology in the pelvis
• The larger patient
For specialized surgeons with extra training these are not limitations as most of these excuses can be overcome by the use of minimal access techniques.
Questions women should ask before undergoing a hysterectomy would be:
• The training credentials of her surgeon
• Whether her ovaries should be removed at the same time (in most cases they do not need to be removed)
• Whether their cervix need to be removed
If women have had normal cervical smears and are in a cervical screening program there is no absolute need for the cervix to be removed.
In Dasmahapatras practice the primary route of hysterectomy for 99% of patients is laparoscopic (keyhole) hysterectomy as this is associated with the least risk of complications, shorter hospital stay, less pain and an earlier return to normal activities.
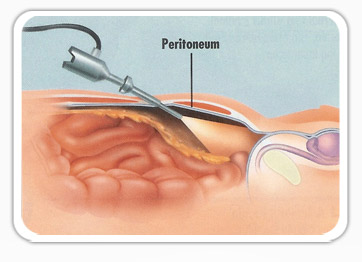
Laparoscopic surgery also known as keyhole surgery is one of the greatest modern advances of gynaecological surgery and today most gynaecological procedures can be performed with key hole surgery.
It involves passing a small camera through the belly button to visualise and operate on pelvic and abdominal contents using very small incisions with the surgeon looking at a monitor. It is associated with less tissue trauma thus less scarring, less pain, less blood loss, quicker discharge from hospital, earlier recovery and quicker return to normal activity.
Laparoscopy can now be used to manage fibroids (in some cases large and m
ultiple fibroids), Endometriosis, ovarian cysts, ectopic pregnancy, adhesions, chronic pelvic pain and a range of other illnesses it can also be used to reverse sterilisation.
Surgeons need to be highly skilled to perform effective and complication free minimal access surgery, particularly for advanced and complicated procedures.
Another form of minimal access surgery is a hysteroscopy. In this case, the tiny camera is inserted into the womb through the vagina. This is another very effective technique which is, once again, less traumatic than conventional surgery.
Dr Dasmahapatra is a highly skilled and formally trained advanced minimal access surgeon who is able to provide minimal access surgery for most routine and complicated gynaecological complaints.
Female sterilization is the most effective form of contraception. At the time of sterilization women are warned of the potential irreversibility of the procedure, however life circumstances change and women may desire more children.
There are two ways of achieving pregnancy after sterilization: either assisted conception methods like IVF or reversal of sterilization. The difference between the two is that women would have to pay for each conception cycle whereas if the reversal of sterilization is successful it is possible to use it more than once.
Historically reversal of sterilization used to be undertaken by conventional open surgery using microsurgical principles. It is now possible to achieve the same results with a laparoscopic procedure.
The success rates for reversal vary from 47-80% the success rates sometimes depend on the type of sterilization that was performed, the extent of the tube that was removed or damaged or if it was carried out at caesarean section.
Other factors that affect success would be the age of the woman seeking reversal (as fertility declines naturally after the age of 35) of sterilization and the presence of any other pathology.
It is also important to ensure that the male partner has a semen sample that is adequate for pregnancy.
The operation itself is carried out laparoscopically with additional incisions on each side of the pelvis just above the pubic hair line, the procedure is usually completed in an hour or 90 minutes and patients are able to go home the same day or after an overnight stay.
The main thing to be aware of after the reversal procedure is the risk of ectopic pregnancy.
Ovarian cysts are “growths” on the ovary which are often fluid filled sacs. The majority of these cysts are benign and often require no intervention, as most will resolve spontaneously in 6 months
They are commonest in the reproductive years and can be broadly classified into 2 groups
• Functional ovarian cysts. These are usually harmless and are a consequence of the normal female menstrual cycle
• Pathological ovarian cysts. These are less common and are as a consequence of abnormal growths within the ovary
The majority of pathological ovarian cysts are benign particularly in the reproductive years.
Because of complications that can occur with ovarian cysts they are the 4th most common reason for acute gynaecological admission, by the age of 65 years 4% of women would have been admitted to hospital for this reason.
The majority of pathological ovarian cysts are benign particularly in the reproductive years.
Because of complications that can occur with ovarian cysts they are the 4th most common reason for acute gynaecological admission, by the age of 65 years 4% of women would have been admitted to hospital for this reason.
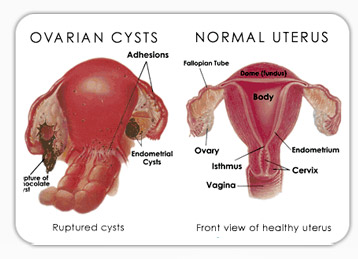
Worrisome complications include-
• Ovarian torsion: this is where the ovary twists on itself, deprives itself of blood supply and causes acute onset of abdominal pain.
• Bleeding from the ovary: if the bleeding is not arrested spontaneously this also can be a cause of acute abdominal pain
• Infection;
• Rupture: this is where the contents of the cyst rupture and are spilled into the abdomen and cause irritation and pain
• Risk of Cancer: the risk of ovarian cancer is rare and to help differentiate between this and benign disease, gynaecologists rely on history, scan findings and special blood tests.
The diagnosis of ovarian cysts and most often their nature is determined by pre-operative investigations which include a pelvic ultrasound scan, which is most often performed vaginally. This is coupled with blood tests most often a Ca125 test. This test in itself is non specific but can on occasion point to the nature of the cyst.
Cysts less than 5cm are often treated conservatively without operation and a follow-up scan organized for 6 weeks after the first. Larger cysts or cysts that cause pain or of a suspicious nature often require surgery.
The main worry in the management of ovarian cysts is to make sure that cancer is not missed and accurate diagnosis is made before surgery. And if surgery is required, as most women are in their reproductive years fertility sparing procedures are carried out and herein lies the beauty of laparoscopic surgery in the management of ovarian cysts.
Size alone is not a limitation to the management of ovarian cysts by laparoscopy as “giant” ovarian cysts can be managed by laparoscopy with the right surgical skills.
Chronic pelvic pain is defined as intermittent or constant pain in the pelvis or lower abdomen of at least 6 months duration. It is as common as migraine and low back pain. It affects about 1 in 6 of the female population.
Pain by definition is a sensory and emotional experience associated with actual or potential tissue damage, it is an individual experience and can be affected by physical, psychological and social factors. The source can be difficult to find on occasion as sometimes even when the provoking factor is removed the pain still occurs.
The aim of management of pelvic pain is to effect diagnosis in a short a time as possible and institute treatment to improve quality of life. Careful scrutiny of the woman’s history and a careful physical exam are essential to try and locate the source of pain
Because of the number of organs in the pelvis the origin of pain my be in the gynaecological organs, or the bladder or bowel or may be as a result of irritation or damage of bones, muscles or nerves.

Common causes include:
1) Gynaecological -
• Endometriosis
• Adenomyosis
• Pelvic inflammatory disease (infection)
• Pelvic adhesions (scar tissue)
2) Gastrointestinal (bowel related)-
• Irritable bowel syndrome
3) Genito-urinary (bladder related)-
• Interstitial cystitis
4) Musculoskeletal (related to muscle or bones)
5) Nerve entrapment
6) Psychological and social issues
One of the most important requirements for diagnosis is the gynaecologists ability to listen and examine as taking a full history may take time, symptoms should not just be put down to psychological issues in the first instance and symptoms should not be dismissed. The woman should also understand that because of the nature of chronic pelvic pain actual diagnosis may take a while and the source of pain may never be found. If the latter were the case then it would be a matter of managing the pain symptoms in the absence of an actual diagnosis.
Investigations will depend on the history and examination and what system of the body is thought to be involved. Commonly an ultrasound will be arranged. Laparoscopy is usually a second line investigation. A laparoscopy is the only test that is capable of diagnosing peritoneal endometriosis or adhesions. Women should not be disappointed if the laparoscopy is negative as though this excludes visual pathology it does not mean that the pain experienced is not real. And some women tend to get better even though nothing is found at laparoscopy.
This is defined as vaginal bleeding 1 year after cessation of menstruation.
Should women have bleeding one year after the menopause they need to visit their doctor.
There are a number of reasons why women might bleed after the menopause and the majority of them are benign and not life threatening but why doctors are worried is because of the possibility of Endometrial Cancer (Cancer of the womb).
When endometrial cancer is caught early is it potentially completely curable. This is the reason why early diagnosis is the key.
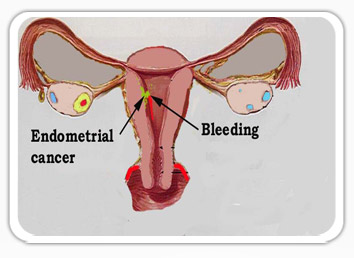
The following increase your risk of endometrial cancer:
• Diabetes
• Estrogen replacement therapy without the use of progesterone
• History of endometrial polyps or other benign growths of the uterine lining
• Infertility (inability to become pregnant)
• Infrequent periods
• Tamoxifen, a drug for breast cancer treatment
• Never being pregnant
• Obesity
• Polycystic ovarian syndrome (PCOS)
• Starting menstruation at an early age (before age 12)
• Starting menopause after age 50.
Consultation will involve a detailed history and examination. For some women it is possible to take a sample of the endometrium (the lining of the womb) with a small tube at the index consultation.
For others it may be that once the history is taken an ultrasound scan is arranged (this is often transvaginal) to assess the thickness of the lining of the womb. The rule of thumb is that if it is greater than 5mm further investigation is required.
The next investigation would be a hysteroscopy where as small camera is put into the womb and a sample taken from the lining, once again it is possible to do this in an outpatient setting without the need for general anaesthesia.
PMS is a collection of physical and behavior and emotional symptoms related to a woman's menstrual cycle, in the absence of any physical or psychiatric illness. The degree of distress and symptoms vary from woman to woman. It occurs in 3-30% of women it is more prevalent in obese women and those who do not undertake exercise. There is a lower incidence in women who use the oral contraceptive pill.
The exact cause of this syndrome is unknown. There is no one specific test for diagnosis and no single treatment.

Management:
Lifestyle alteration, both diet and exercise help as does stress management and cognitive behavioural therapy. Sometimes the oral contraceptive pill can be used as first line therapy. Low dose antidepressants are also used on the days when symptoms are severe leading up to the menstrual cycle.
Second line treatment includes the use of the Mirena intrauterine contraceptive device and other forms of hormonal manipulation. Sometimes higher doses of anti-depressants are required.
If this doesn’t work hormone implants may be of benefit to suppress the function of the ovaries. The ultimate treatment is removal of the ovaries coupled with hormone replacement therapy. This should only be done as a last resort and in women whose family is complete and after all other treatments fail. Sometimes women are advised to have a trial with hormone therapy to suppress the ovaries before surgery to ascertain whether they would benefit from the procedure.
This is a female disorder, though the exact cause is unknown it is thought to be due to hormonal imbalance. It is a complex endocrine abnormality that usually begins in puberty and is common during the reproductive years, producing symptoms in about 5-10% of women.
The principal features are due to:
• Anovulation (not producing an “egg” each month) resulting in irregular or absent menstrual periods.
• Hyperandrogenism: there is also a production of androgenic (male) hormones that is responsible for acne, hirsuitism (abnormal hair growth),
• Insulin resistance: PCO is associated with obesity, type 2 diabetes and sometimes high cholesterol levels.
• Infertility: It is thought to be one of the leading causes of sub-fertility.
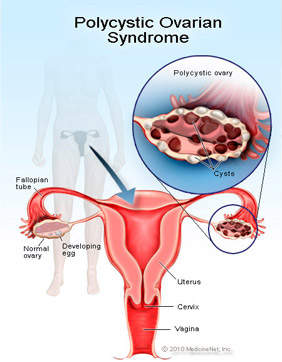
Not all women will have all symptoms, the severity and the type of symptoms vary greatly among affected individuals.
Consultation usually involves a detailed history looking at menstrual patterns, abnormal hair growth and body mass index (weight and height).
After a physical examination the first investigation is usually an ultrasound scan (preferably a transvaginal scan) this is done to look at the ovaries which have certain characteristics in women with PCOS, the so called “string of pearl” appearance.
Other investigations are usually blood tests looking at various hormone levels on certain days of the menstrual cycle.
Management centers on managing the symptoms. It centers around understanding the syndrome and individualising treatment by
• Restoring fertility if desired
• Lowering insulin levels
• Treatment of hirsutim and acne
• Restoration of regular menstruation
For the overweight woman, diet coupled with exercise is first tried and if weight is lost and the BMI is improved periods can regularise themselves spontaneously.
Medication centers on improving insulin resistance by means of a drug called Metformin, in some cases the oral contraceptive pill is given to regulate periods particularly if fertility is not an immediate issue.
When fertility is the main issue treatment is concentrated on weight loss, improving insulin resistance with Metformin and induction of ovulation. The commonest drug for this is clomiphene citrate.
For hirsuitism and acne the oral contraceptive pill is used. There are also other medications that can be used for the unwanted hair growth.
In extreme cases laparoscopy may be necessary if medication fails and a procedure called laparoscopic ovarian drilling. Here during the laparoscopy little holes are made in the ovary to reduce the number of follicles. It is usually performed as a day case procedure
PCOS can be transient and in those individuals in whom symptoms improve they should actually adopt life-styles that will prevent the development of diabetes.
Pelvic floor disorders include prolapse of the womb or parts of the vagina, incontinence of urine and sometimes incontinence of faeces.
The life time risk of women undergoing surgery for prolapse or incontinence is about 11%. About 50% of women who have had children will develop prolapse. And more women will develop prolapse as life expectancy is increased, but not all will require intervention.
Factors that can influence the development of prolapse include: childbearing, the menopause, occupational stresses that put pressure on the pelvic floor, constipation, chronic cough as well as surgery on the pelvic floor, particularly hysterectomy. The cumulative risk of development of prolapse after hysterectomy is 1% at 3 years and 5% at 15 years the risk is 5.5% higher if hysterectomy is performed for prolapse.
As with all conditions in gynaecology it is important to have a holistic approach to management. A detailed history and examination need to be carried out taking into account the patients circumstance and whether family is complete or not. This is because there is a failure risk with surgery and the risk of recurrence can be as high as 30% in some cases.
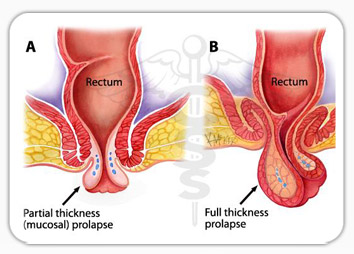
Before surgery is offered it may be possible to adopt a conservative approach with pelvic floor exercises or the use of pessaries (devices that are able to support the pelvic floor when inserted into the vagina). These can be particularly useful for women who have not completed their families and for those due to medical complaints are not able to have surgery.
Surgery for pelvic floor prolapse has evolved overtime and there are numerous operations some of which have not stood the test of time. Before surgery is undertaken depending on the part of the vagina that has prolapsed it may be necessary to carry out investigations such as urodynamics to see how the bladder functions and how it may be affected by surgery.
For “vault” prolapse after hysterectomy one of the commonest operations offered is a Sacrocolpopexy. These days this is most often performed laparoscopically. It is superior to most vaginal approaches. Another operation called a sacrohysteropexy ( where the womb is left in place despite prolapse) is also performed laparoscopically and is offered to women who do not want to have a hysterectomy or those where the womb has prolapsed and but have not completed their family.
Sacrospinous fixations are operations performed vaginally for the same prolapse but failure rates are higher.
In recent years there have been a proliferation of “Meshes” used for vaginal surgery repair. The theory behind their use is because of the high recurrence risk with vaginal surgery for prolapse repair. Vaginal mesh surgery needs to be approached with caution because of the risk of Mesh erosion and other complications. The advice is that most women will not require mesh for a first vaginal prolapse operation and should only need it if prolapse recurs after surgery.
Unlike the use of meshes for vaginal repair, for urinary incontinence the use of mesh is the way forward and has replaced conventional surgery for most women who suffer from stress incontinence.
dr mahapatra is able to offer a structured and holistic approach to the management of women with pelvic floor disorders and incontinence. With minimal access surgical approach in most cases.
Urinary incontinence is defined as involuntary loss of urine. It is generally divided into 2 main types:
1. Stress incontinence: which is the involuntary loss of urine on coughing or sneezing or on exercise and
2. Overactive bladder: which is the inability to hold on to urine when one has the urge to go
Overactive bladder is characterised by:
• Frequency
• Urgency
• Nocturia
• Urge incontinence
3. Mixed incontinence: Some women have both symptoms and this is known as mixed incontinence
Incontinence of urine unfortunately is under reported probably due to the embarrassment it causes the sufferer. Putting it in perspective 1:7 women over the age of 30 suffer from some form of incontinence and about 2.5 million women suffer with this problem in the UK, however up to 88% of women suffer for a year or more before seeking medical help, with 46% of women suffering for up to 5 years before they seek medical help.
For women who seek medical help it is once again important to take a detailed history and examination, trying to differentiate between the types of incontinence. If the diagnosis cannot be reached on the basis of history alone it may be necessary for the woman to keep a urinary diary for a few days to help in the analysis.
For women with overactive bladder symptoms it is best to try conservative measures first. This is usually in the form of bladder re-education carried out either by a physiotherapist of an incontinence advisor. Alterations in life style may also be advised: avoidance of coffee and other stimulants may be helpful. Some may be advised to try cranberry juice.
If this doesn’t work then medication may be necessary this is usually in the form of an anticholinergic agent. The efficacy of anticholinergic agents is sometimes limited by their side effects, which include blurred vision, constipation and dry mouth. Some women may need to switch from one drug to another till they find the one that suits them.
When diagnosis is inconclusive it may be necessary to perform a test called urodynamics. During this test a catheter (a little tube) is inserted into the bladder and the bladder if filled with fluid and recordings are taken on a computer looking at how the bladder reacts to filling.
For women with pure stress incontinence treatment is initially conservative in the form of pelvic floor exercises supervised by an incontinence advisor or physiotherapist. There are also come devices that can be inserted into the vagina to prevent incontinence (this may be helpful for athletes or when a woman needs to undertake strenuous activity for a short period of time). If this fails then surgery may be necessary. The commonest procedure performed today for urinary incontinence is the tension free transvaginal tape either suprapubic or trans-obturator. The success rate of this procedure is about 95-97%.
Complications include needing to go to the toilet more often in about 10% of women who have the procedure, difficulty in voiding in about 10% of women. The mesh used for the procedure may erode in about 3-8% of women. Other complications include bladder injury, painful intercourse for the woman and painful intercourse for the partner if the mesh used erodes (His-pareunia).
Other therapies are also available depending on the patients individual circumstances e.g. Bulking agents or some times relatively complex surgery.
The best approach to the management of incontinence is a multi-disciplinary approach and best managed in a caring environment within the woman’s own community only needing to see a specialist if conservative measures fail.